Editor's Note -
One of the clearest and most concise sources of information about "Medicare for All" and for the cases for and against it
I've seen is a newly published pamphlet, the latest in a series by Dr. John Geyman. He has modeled it after the famous series of pamphlets written by Thomas Paine in the 18th century regarding American Independence.
It is titled "Common Sense: The Case For And Against Medicare For All - Leading Issue in the 2020 Elections."
In it, he discusses:
What is Single-Payer Medicare for All!
The Case for Expanded & Improved Medicare for All
The Case against Medicare for All, including rebuttal of Myths
How Should We Decide?
Useful Resources
It will take you about 15 minuters to read and is available from Amazon for $5.95. Here is the link to it.
https://www.amazon.com/Common-Sense-Case-Against-Medicare/dp/193821823X/ref=sr_1_1?crid=1FPJBLGVA6DBI&keywords=common+sense+the+case+for+and+against+medicare+for+all&qid=1560946363&s=gateway&sprefix=common+sense+the+case+%2Caps%2C162&sr=8-1
-SPC
Trump Wants to Neutralize Democrats on Health Care. Republicans Say Let It Go.
By Peter Baker, Michael Tackett and Linda Qiu - NYT - June 16, 2019
WASHINGTON — As President Trump prepares to kick off his
bid for a second term this week, he is anxiously searching for a way to
counter Democrats on health care, one of their central issues, even
though many of his wary Republican allies would prefer he let it go for
now.
Since he announced his previous run four years ago, Mr. Trump has promised to replace President Barack Obama’s health care law with “something terrific” that costs less and covers more without ever actually producing such a plan.
Now he is vowing to issue the plan within a month or two, reviving a campaign promise with broad consequences for next year’s contest. If he follows through, it could help shape a presidential race that Democrats would like to focus largely on health care.
While the president has acknowledged that no plan would be voted on in Congress until 2021, when he hopes to be in a second term with Republicans back in charge of the House, he is gambling that putting out a plan to be debated on the campaign trail will negate some of the advantage Democrats have on the issue.
Since he announced his previous run four years ago, Mr. Trump has promised to replace President Barack Obama’s health care law with “something terrific” that costs less and covers more without ever actually producing such a plan.
Now he is vowing to issue the plan within a month or two, reviving a campaign promise with broad consequences for next year’s contest. If he follows through, it could help shape a presidential race that Democrats would like to focus largely on health care.
While the president has acknowledged that no plan would be voted on in Congress until 2021, when he hopes to be in a second term with Republicans back in charge of the House, he is gambling that putting out a plan to be debated on the campaign trail will negate some of the advantage Democrats have on the issue.
But
nervous Republicans worry that putting out a concrete plan with no
chance of passage would only give the Democrats a target to pick apart
over the next year. The hard economic reality of fashioning a plan that
lives up to the promises Mr. Trump has made would invariably involve
trade-offs unpopular with many voters.
“Obamacare has been a disaster,” Mr. Trump told ABC News in an interview aired on Sunday evening. His own plan, he insisted, would lower costs. “You’ll see that in a month when we introduce it. We’re going to have a plan. That’s subject to winning the House, Senate and presidency, which hopefully we’ll win all three. We’ll have phenomenal health care.”
The president’s renewed interest in health care comes as he plans an elaborate rally in Orlando, Fla., on Tuesday to open a re-election campaign that is already struggling to find its bearings. After last week’s leak of a series of dismal internal poll results from March showing him trailing in multiple battleground states, Mr. Trump first denied that the surveys even existed, only to have his campaign later confirm that they in fact were real.
By Sunday, the episode had led to a purge as the Trump campaign indicated that it would cut ties with three of its five pollsters, a sign of internal discord in an operation seeking to be far more organized and professional than the slapdash, one-man show that Mr. Trump ran out of Trump Tower in New York four years ago.
Democratic leaders have argued that they won control of the House in last year’s midterm elections in large part on the health care issue, and they have been pressing the point in recent weeks. Over the weekend, 140 House Democrats, more than half of the party’s caucus, held events or online town halls to talk about health care, their largest coordinated action in districts since winning the majority.
“Obamacare has been a disaster,” Mr. Trump told ABC News in an interview aired on Sunday evening. His own plan, he insisted, would lower costs. “You’ll see that in a month when we introduce it. We’re going to have a plan. That’s subject to winning the House, Senate and presidency, which hopefully we’ll win all three. We’ll have phenomenal health care.”
The president’s renewed interest in health care comes as he plans an elaborate rally in Orlando, Fla., on Tuesday to open a re-election campaign that is already struggling to find its bearings. After last week’s leak of a series of dismal internal poll results from March showing him trailing in multiple battleground states, Mr. Trump first denied that the surveys even existed, only to have his campaign later confirm that they in fact were real.
By Sunday, the episode had led to a purge as the Trump campaign indicated that it would cut ties with three of its five pollsters, a sign of internal discord in an operation seeking to be far more organized and professional than the slapdash, one-man show that Mr. Trump ran out of Trump Tower in New York four years ago.
Democratic leaders have argued that they won control of the House in last year’s midterm elections in large part on the health care issue, and they have been pressing the point in recent weeks. Over the weekend, 140 House Democrats, more than half of the party’s caucus, held events or online town halls to talk about health care, their largest coordinated action in districts since winning the majority.
In particular, Democrats hammered the Trump administration for asking a court in March to overturn the entire Affordable Care Act,
which among other things would eliminate protections for patients with
pre-existing conditions. Mr. Trump has repeatedly said he favors such
protections but has not explained how he would achieve them if the
Obama-era law were invalidated.
“The Trump administration is currently suing to eliminate the law that guarantees health care coverage for Americans with pre-existing conditions,” said Representative Ted Lieu of California, a leader of the Democratic committee that organized the weekend activities. “That action speaks for itself. If Trump wants to be serious about health care, he needs to stop the lawsuit and his other actions that seek to sabotage the A.C.A.”
While House Democrats advance incremental measures on health care, some prominent liberals, including presidential candidates like Senator Bernie Sanders of Vermont, have proposed a single-payer government-run health care plan that they call “Medicare for all,” hoping to capitalize on the popularity of the program for the elderly by expanding it to the population at large.
Mr. Trump and other Republicans see that as an opening for them on the campaign trail by characterizing it as socialism. Such a huge shift in how health care is run in the United States would not only put the government in charge, they say, but also cost enormous amounts of taxpayer money and force Americans to give up private insurance coverage they might like.
Mr. Sanders was pressed on those criticisms during an appearance on “Fox News Sunday” and argued that the current system was unsustainable, implicitly offering his own criticisms of the program erected by Mr. Obama from the left.
When
they were in the majority, House Republicans voted dozens of times to
repeal the Affordable Care Act, also known as Obamacare, only to see
their legislation die in the Senate. On one occasion, Mr. Trump summoned
House Republicans to the White House for a grand ceremony only to see
that momentum quickly fade away.
Mr. Trump often laments the failure by blaming Senator John McCain, Republican of Arizona, who voted against one repeal effort in the summer of 2017. Even if Mr. McCain had voted for the bill, however, full repeal of the Affordable Care Act would not have been assured.
That version would have eliminated the individual and employers’ mandate, but left intact the health care law’s Medicaid expansion and insurance regulations. And it would still have required passage in the House or forced lawmakers from both chambers to negotiate their differences.
When Mr. Trump pushed the idea of voting to repeal the law again recently, he was quickly dissuaded by Senator Mitch McConnell, Republican of Kentucky and the majority leader, who argued that comprehensive health care legislation would go nowhere in Congress. The president then insisted it was never his intention to vote on a bill before the 2020 election.Even as Mr. Trump has delayed producing a plan, he has continued to criticize the existing health care law, repeatedly claiming that it had become unaffordable because of average deductibles exceeding $7,000 or $8,000. This was an exaggeration.
Deductibles vary greatly by the type of plan and the enrollee. While deductibles for some plans can top $7,000, they average $4,375 for silver-tier plans, the most common choice for consumers. And those who receive cost-sharing reductions have lower deductibles still. Also left unsaid was his own administration’s role in causing higher deductibles, as the federal government sets caps on out-of-pocket costs and has increased the limit this year.
Midway through his third year in office, many remain skeptical that Mr. Trump will produce the plan he is now promising to unveil in a month or two.
“He can’t deliver the impossible,” said Len M. Nichols, the director of the Center for Health Policy Research and Ethics at George Mason University, “so he avoids specifics and postpones actually reckoning with a serious legislative proposal of his own.”
https://www.nytimes.com/2019/06/16/us/politics/trump-health-care-democrats-2020.html?smid=nytcore-ios-share
“The Trump administration is currently suing to eliminate the law that guarantees health care coverage for Americans with pre-existing conditions,” said Representative Ted Lieu of California, a leader of the Democratic committee that organized the weekend activities. “That action speaks for itself. If Trump wants to be serious about health care, he needs to stop the lawsuit and his other actions that seek to sabotage the A.C.A.”
While House Democrats advance incremental measures on health care, some prominent liberals, including presidential candidates like Senator Bernie Sanders of Vermont, have proposed a single-payer government-run health care plan that they call “Medicare for all,” hoping to capitalize on the popularity of the program for the elderly by expanding it to the population at large.
Mr. Trump and other Republicans see that as an opening for them on the campaign trail by characterizing it as socialism. Such a huge shift in how health care is run in the United States would not only put the government in charge, they say, but also cost enormous amounts of taxpayer money and force Americans to give up private insurance coverage they might like.
Mr. Sanders was pressed on those criticisms during an appearance on “Fox News Sunday” and argued that the current system was unsustainable, implicitly offering his own criticisms of the program erected by Mr. Obama from the left.
“You have a dysfunctional health care system,” he said. “You’ve
got 70 million Americans who either have no health insurance or they are
underinsured with high deductibles and co-payments. We are paying twice
as much as any other country on earth for the prescription drugs that
we need. We spend far more per capita on health care as do the people of
any other country.”
Democrats enjoy a strong edge
with voters on health care, with 40 percent trusting them on the issue,
compared with 23 percent who trust Republicans more, according to an April poll by The Associated Press and the NORC Center for Public Affairs Research.
Forty-two percent of Americans in that survey favored a single-payer system along the lines of what Mr. Sanders is proposing, while 31 percent opposed it and 25 percent did not take a position. Views of the Affordable Care Act are split right down the middle, with 50 percent approving of it and 48 percent disapproving of it in an April poll by Gallup.
Given the Democratic advantage, many Republicans say they should not focus their energy on health care but instead emphasize immigration and other issues where they are stronger. But the president and his team counter that even if they cannot win on health care, it would be ridiculous to simply cede the territory if they could at least narrow the gap.
The president feels compelled to have something specific to counter Medicare for all. Still, people close to Mr. Trump suggested that if he did release something within a month or two, it might not be a comprehensive plan but a series of smaller proposals that would potentially help, such as ideas for bringing down prescription drug costs, for giving states more flexibility on Medicaid expansion and for promoting more access in the marketplace.
Among those who are said to be influencing the discussion within the administration are Alex M. Azar II, the secretary of health and human services; Seema Verma, the head of the agency that runs Medicare and Medicaid; and Joe Grogan, the director of the White House Domestic Policy Council.
“The president has repeatedly promised something better than the A.C.A. but has never come up with a plan himself, and the congressional plans he endorsed were definitely not better for everyone,” said Larry Levitt, a senior vice president at the Kaiser Family Foundation.
“There’s always a tension for presidents around whether to submit a specific proposal to Congress or let the legislative process play out,” Mr. Levitt added. “When it comes to health care, the challenge has been that the president has not only avoided proposing a specific plan, but has made promises that no plan could ever fulfill.”
Forty-two percent of Americans in that survey favored a single-payer system along the lines of what Mr. Sanders is proposing, while 31 percent opposed it and 25 percent did not take a position. Views of the Affordable Care Act are split right down the middle, with 50 percent approving of it and 48 percent disapproving of it in an April poll by Gallup.
Given the Democratic advantage, many Republicans say they should not focus their energy on health care but instead emphasize immigration and other issues where they are stronger. But the president and his team counter that even if they cannot win on health care, it would be ridiculous to simply cede the territory if they could at least narrow the gap.
The president feels compelled to have something specific to counter Medicare for all. Still, people close to Mr. Trump suggested that if he did release something within a month or two, it might not be a comprehensive plan but a series of smaller proposals that would potentially help, such as ideas for bringing down prescription drug costs, for giving states more flexibility on Medicaid expansion and for promoting more access in the marketplace.
Among those who are said to be influencing the discussion within the administration are Alex M. Azar II, the secretary of health and human services; Seema Verma, the head of the agency that runs Medicare and Medicaid; and Joe Grogan, the director of the White House Domestic Policy Council.
“The president has repeatedly promised something better than the A.C.A. but has never come up with a plan himself, and the congressional plans he endorsed were definitely not better for everyone,” said Larry Levitt, a senior vice president at the Kaiser Family Foundation.
“There’s always a tension for presidents around whether to submit a specific proposal to Congress or let the legislative process play out,” Mr. Levitt added. “When it comes to health care, the challenge has been that the president has not only avoided proposing a specific plan, but has made promises that no plan could ever fulfill.”
Mr. Trump often laments the failure by blaming Senator John McCain, Republican of Arizona, who voted against one repeal effort in the summer of 2017. Even if Mr. McCain had voted for the bill, however, full repeal of the Affordable Care Act would not have been assured.
That version would have eliminated the individual and employers’ mandate, but left intact the health care law’s Medicaid expansion and insurance regulations. And it would still have required passage in the House or forced lawmakers from both chambers to negotiate their differences.
When Mr. Trump pushed the idea of voting to repeal the law again recently, he was quickly dissuaded by Senator Mitch McConnell, Republican of Kentucky and the majority leader, who argued that comprehensive health care legislation would go nowhere in Congress. The president then insisted it was never his intention to vote on a bill before the 2020 election.Even as Mr. Trump has delayed producing a plan, he has continued to criticize the existing health care law, repeatedly claiming that it had become unaffordable because of average deductibles exceeding $7,000 or $8,000. This was an exaggeration.
Deductibles vary greatly by the type of plan and the enrollee. While deductibles for some plans can top $7,000, they average $4,375 for silver-tier plans, the most common choice for consumers. And those who receive cost-sharing reductions have lower deductibles still. Also left unsaid was his own administration’s role in causing higher deductibles, as the federal government sets caps on out-of-pocket costs and has increased the limit this year.
Midway through his third year in office, many remain skeptical that Mr. Trump will produce the plan he is now promising to unveil in a month or two.
“He can’t deliver the impossible,” said Len M. Nichols, the director of the Center for Health Policy Research and Ethics at George Mason University, “so he avoids specifics and postpones actually reckoning with a serious legislative proposal of his own.”
https://www.nytimes.com/2019/06/16/us/politics/trump-health-care-democrats-2020.html?smid=nytcore-ios-share
Trump Officials Broaden Attack on Health Law, Arguing Courts Should Reject All of It
by Robert Pear - March 25, 2019
WASHINGTON
— The Trump administration broadened its attack on the Affordable Care
Act on Monday, telling a federal appeals court that it now believed the
entire law should be invalidated.
The administration had previously said that the law’s protections for people with pre-existing conditions should be struck down, but that the rest of the law, including the expansion of Medicaid, should survive.
If the appeals court accepts the Trump administration’s new arguments, millions of people could lose health insurance, including those who gained coverage through the expansion of Medicaid and those who have private coverage subsidized by the federal government.
“The Justice Department is no longer asking for partial invalidation of the Affordable Care Act, but says the whole law should be struck down,” Abbe R. Gluck, a law professor at Yale who has closely followed the litigation, said on Monday. “Not just some of the insurance provisions, but all of it, including the Medicaid expansion and hundreds of other reforms. That’s a total bombshell, which could have dire consequences for millions of people.”
The administration had previously said that the law’s protections for people with pre-existing conditions should be struck down, but that the rest of the law, including the expansion of Medicaid, should survive.
If the appeals court accepts the Trump administration’s new arguments, millions of people could lose health insurance, including those who gained coverage through the expansion of Medicaid and those who have private coverage subsidized by the federal government.
“The Justice Department is no longer asking for partial invalidation of the Affordable Care Act, but says the whole law should be struck down,” Abbe R. Gluck, a law professor at Yale who has closely followed the litigation, said on Monday. “Not just some of the insurance provisions, but all of it, including the Medicaid expansion and hundreds of other reforms. That’s a total bombshell, which could have dire consequences for millions of people.”
The new position is
also certain to reignite a political furor over the Affordable Care
Act, ensuring that it will figure even more prominently in the 2020
elections. Democrats have been saying that President Trump still wants
to abolish the law, and they can now point to the Justice Department’s
filing as evidence to support that contention.
[What happens if Obamacare is struck down? Read more.]
The Justice Department disclosed its new stance in a two-sentence letter to the United States Court of Appeals for the Fifth Circuit, in New Orleans, and will elaborate on its position in a brief to be filed later.
In the letter, the Justice Department said the court should affirm a judgment issued in December by Judge Reed O’Connor of the Federal District Court in Fort Worth.
Judge O’Connor, in a sweeping opinion, said that the individual mandate requiring people to have health insurance “can no longer be sustained as an exercise of Congress’s tax power” because Congress had eliminated the tax penalty for people who go without health insurance.
Accordingly, Judge O’Connor said, “the individual mandate is unconstitutional” and the remaining provisions of the Affordable Care Act are also invalid.
[What happens if Obamacare is struck down? Read more.]
The Justice Department disclosed its new stance in a two-sentence letter to the United States Court of Appeals for the Fifth Circuit, in New Orleans, and will elaborate on its position in a brief to be filed later.
In the letter, the Justice Department said the court should affirm a judgment issued in December by Judge Reed O’Connor of the Federal District Court in Fort Worth.
Judge O’Connor, in a sweeping opinion, said that the individual mandate requiring people to have health insurance “can no longer be sustained as an exercise of Congress’s tax power” because Congress had eliminated the tax penalty for people who go without health insurance.
Accordingly, Judge O’Connor said, “the individual mandate is unconstitutional” and the remaining provisions of the Affordable Care Act are also invalid.
In
its letter to the appeals court, the Justice Department said on Monday
that it “is not urging that any portion of the district court’s judgment
be reversed.” In other words, it agrees with Judge O’Connor’s ruling.
In the nine years since it was signed by President Barack Obama, the Affordable Care Act has become embedded in the nation’s health care system. It changed the way Medicare pays doctors, hospitals and other health care providers. It has unleashed a tidal wave of innovation in the delivery of health care. The health insurance industry has invented a new business model selling coverage to anyone who applies, regardless of any pre-existing conditions.
The law also includes dozens of provisions that are less well known and not related to the individual mandate. It requires nutrition labeling and calorie counts on menu items at chain restaurants. It requires certain employers to provide “reasonable break time” and a private space for nursing mothers to pump breast milk. It improved prescription drug coverage for Medicare beneficiaries, and it created a new pathway for the approval of less expensive versions of biologic medicines made from living cells.
Lawyers said invalidation of the entire law would raise numerous legal and practical questions. It is, they said, difficult to imagine what the health care world would look like without the Affordable Care Act.
The Trump administration’s new position was harshly criticized by the insurance industry and by consumer advocates.
The government’s position “puts coverage at risk for more than 100 million Americans,” said Matt Eyles, the president and chief executive of America’s Health Insurance Plans.
Leslie Dach, the chairman of Protect Our Care, a consumer advocacy group, said: “In November, voters overwhelmingly rejected President Trump’s health care repeal and sabotage agenda. But he remains dead set on accomplishing through the courts what he and his allies in Congress could not do legislatively: fully repeal the law, devastate American health care and leave millions of Americans at risk.”
In the nine years since it was signed by President Barack Obama, the Affordable Care Act has become embedded in the nation’s health care system. It changed the way Medicare pays doctors, hospitals and other health care providers. It has unleashed a tidal wave of innovation in the delivery of health care. The health insurance industry has invented a new business model selling coverage to anyone who applies, regardless of any pre-existing conditions.
The law also includes dozens of provisions that are less well known and not related to the individual mandate. It requires nutrition labeling and calorie counts on menu items at chain restaurants. It requires certain employers to provide “reasonable break time” and a private space for nursing mothers to pump breast milk. It improved prescription drug coverage for Medicare beneficiaries, and it created a new pathway for the approval of less expensive versions of biologic medicines made from living cells.
Lawyers said invalidation of the entire law would raise numerous legal and practical questions. It is, they said, difficult to imagine what the health care world would look like without the Affordable Care Act.
The Trump administration’s new position was harshly criticized by the insurance industry and by consumer advocates.
The government’s position “puts coverage at risk for more than 100 million Americans,” said Matt Eyles, the president and chief executive of America’s Health Insurance Plans.
Leslie Dach, the chairman of Protect Our Care, a consumer advocacy group, said: “In November, voters overwhelmingly rejected President Trump’s health care repeal and sabotage agenda. But he remains dead set on accomplishing through the courts what he and his allies in Congress could not do legislatively: fully repeal the law, devastate American health care and leave millions of Americans at risk.”
The Trump
administration’s new stance appears to put Republicans in Congress in an
awkward position. They have repeatedly tried to repeal the health law.
But in the last year, they said over and over that they wanted to
protect coverage for people with pre-existing conditions, and those
protections are among the law’s most popular provisions.
The lawsuit challenging the Affordable Care Act, Texas v. United States, was filed last year by a group of Republican governors and state attorneys general. Officials from California and more than a dozen other states have intervened to defend the law.
The Texas lawsuit “is as dangerous as it is reckless,” Xavier Becerra, the attorney general of California, said on Monday as he filed a brief urging the appeals court to uphold the law.
https://www.nytimes.com/2019/03/25/us/politics/obamacare-unconstitutional-trump-aca.html?smid=nytcore-ios-share
The lawsuit challenging the Affordable Care Act, Texas v. United States, was filed last year by a group of Republican governors and state attorneys general. Officials from California and more than a dozen other states have intervened to defend the law.
The Texas lawsuit “is as dangerous as it is reckless,” Xavier Becerra, the attorney general of California, said on Monday as he filed a brief urging the appeals court to uphold the law.
https://www.nytimes.com/2019/03/25/us/politics/obamacare-unconstitutional-trump-aca.html?smid=nytcore-ios-share
On the Doorstep With a Plea: Will You Support Medicare for All?
by Abby Goodnough - NYT - June 15, 2019
DUBUQUE, Iowa — Art Miller listened patiently as the stranger on his doorstep tried to sell him on the Medicare for All Act of 2019, the single-payer health care bill that has sharply divided Democrats in Congress and on the presidential campaign trail.
The visitor, Steven Meier, was a volunteer canvasser who wanted Mr. Miller to call his congresswoman, Abby Finkenauer, the young Democrat who took a Republican’s seat last year in this closely divided district — and press her to embrace Medicare for all. Beyond congressional politics, there was the familiar role that Iowa plays as the first state to weigh in on the fight for the Democratic presidential nomination.
“I want to know how my grandkids are going to pay for it, O.K.?” Mr. Miller, 71, mused, peering at the flier that Mr. Meier had handed him.
It was a fairly typical encounter for Mr. Meier, 39, who with hundreds of volunteers around the country is working with National Nurses United, the country’s largest nurses’ union, to build grass-roots support for the single-payer bill, a long shot on Capitol Hill and a disruptive force in the party. House Democrats have declared this Saturday and Sunday to be “a weekend of action on health care” — but they are split over whether to embrace extreme change or something closer to the status quo.
The visitor, Steven Meier, was a volunteer canvasser who wanted Mr. Miller to call his congresswoman, Abby Finkenauer, the young Democrat who took a Republican’s seat last year in this closely divided district — and press her to embrace Medicare for all. Beyond congressional politics, there was the familiar role that Iowa plays as the first state to weigh in on the fight for the Democratic presidential nomination.
“I want to know how my grandkids are going to pay for it, O.K.?” Mr. Miller, 71, mused, peering at the flier that Mr. Meier had handed him.
It was a fairly typical encounter for Mr. Meier, 39, who with hundreds of volunteers around the country is working with National Nurses United, the country’s largest nurses’ union, to build grass-roots support for the single-payer bill, a long shot on Capitol Hill and a disruptive force in the party. House Democrats have declared this Saturday and Sunday to be “a weekend of action on health care” — but they are split over whether to embrace extreme change or something closer to the status quo.
A single-payer health care system
would more or less scrap private health insurance, including
employer-sponsored coverage, for a system like Canada’s in which the
government pays for everyone’s health care with tax dollars. Democrats
not ready for that big a step are falling back on a “public option,” an
alternative in which anyone could buy into Medicare or another public
program, or stick with private insurance — a position once a considered
firmly on the party’s left wing.
Lawmakers like Ms. Finkenauer, mindful of the delicate political balance in their districts, fear the “socialism” epithet that President Trump and his party are attaching to Medicare for all. On Friday, Mr. Trump called the House bill “socialist health care” that would “crush American workers with higher taxes, long wait times and far worse care.” But even Ms. Finkenauer, who beat the incumbent Republican in November by 16,900 votes, has been pulled left by the debate, embracing the public option, which could not get through Congress when the Affordable Care Act passed in 2010.
Lawmakers like Ms. Finkenauer, mindful of the delicate political balance in their districts, fear the “socialism” epithet that President Trump and his party are attaching to Medicare for all. On Friday, Mr. Trump called the House bill “socialist health care” that would “crush American workers with higher taxes, long wait times and far worse care.” But even Ms. Finkenauer, who beat the incumbent Republican in November by 16,900 votes, has been pulled left by the debate, embracing the public option, which could not get through Congress when the Affordable Care Act passed in 2010.
Mr.
Meier, along with hundreds of other volunteers around the country, is
working with National Nurses United, the country’s largest nurses’
union, to build grass-roots support for the single-payer bill.CreditLauren Justice for The New York Times
“In a divided Congress, I’m focused on what we can do to bring immediate relief to Iowans,” she said in an email.
The nurses’ union and a number of other progressive groups want nothing less than a government system that pays for everyone’s health care, seizing on the issue’s prominence and a round of Medicare for all hearings in the House with canvassing in the districts of many of the 123 House Democrats who have not thrown their support behind a single-payer system.
The nurses’ union and a number of other progressive groups want nothing less than a government system that pays for everyone’s health care, seizing on the issue’s prominence and a round of Medicare for all hearings in the House with canvassing in the districts of many of the 123 House Democrats who have not thrown their support behind a single-payer system.
“Hearings
are a moment for us to have a national stage for this campaign,”
Jasmine Ruddy, the lead organizer for the nurse union’s Medicare for all
campaign, told several dozen new volunteers on a training call last
month. “It’s up to us to take advantage of the momentum we already see
happening and turn it into political power.”
But building support for a single-payer health care system has been slow going. On Wednesday, the chairman of the Ways and Means Committee, Representative Richard E. Neal of Massachusetts, convening the House’s third Medicare for all hearing, said it was about “exploring ideas.”
Republicans warned darkly of sky-high tax increases, doctor shortages and long waits for care. Representative Kevin Brady of Texas, the senior Republican on the committee, said his constituents were “frightened” about their private coverage being “ripped out from under them.”
The nurses’ union campaign began just after Democrats won the House in November, when the union and several other groups held a strategy call with Representative Pramila Jayapal, Democrat of Washington, the chief author of the Medicare for All Act, and Senator Bernie Sanders of Vermont, who pushed Medicare for all into the mainstream during his 2016 presidential campaign.
“Rather than try to convince people it’s the right system,” Ms. Ruddy said, “our strategy is to reach the people who are already convinced that health care is a human right, to bring them in and actually make them feel the action they are taking matters.”
But building support for a single-payer health care system has been slow going. On Wednesday, the chairman of the Ways and Means Committee, Representative Richard E. Neal of Massachusetts, convening the House’s third Medicare for all hearing, said it was about “exploring ideas.”
Republicans warned darkly of sky-high tax increases, doctor shortages and long waits for care. Representative Kevin Brady of Texas, the senior Republican on the committee, said his constituents were “frightened” about their private coverage being “ripped out from under them.”
The nurses’ union campaign began just after Democrats won the House in November, when the union and several other groups held a strategy call with Representative Pramila Jayapal, Democrat of Washington, the chief author of the Medicare for All Act, and Senator Bernie Sanders of Vermont, who pushed Medicare for all into the mainstream during his 2016 presidential campaign.
“Rather than try to convince people it’s the right system,” Ms. Ruddy said, “our strategy is to reach the people who are already convinced that health care is a human right, to bring them in and actually make them feel the action they are taking matters.”
Students
from the Rush University Medical Center demonstrated in support of
Medicare for All legislation outside the Blue Cross Blue Shield of
Illinois headquarters in Chicago.CreditJoshua Lott for The New York Times
In
Dubuque, Mr. Meier and his partner, Briana Moss, have knocked on 250
doors and gathered about 50 signatures over the past few months. About
20 volunteers, including a retired nurse and several college students,
are also involved. Nationwide, canvassers have knocked on 20,000 doors
and collected 14,000 signatures since February.
On
a Saturday afternoon, Mr. Miller, a Vietnam veteran, told Mr. Meier
about his positive experience with government health care through the
Department of Veterans Affairs, saying, “I’ve seen how it can work.”
A few houses down, a woman who owns a cleaning service and would give only her first name, Sharon, and her party affiliation, Republican, said that if the bill covered abortions, “I won’t go for that.”
She added that she would be happy to stop paying $170 a month for supplemental insurance to cover what Medicare does not, but she did not want to see people who do not work receive free care. From the garage, her husband hollered that he agreed. Conceding defeat, Mr. Meier and Ms. Moss moved along.
Both Sanders supporters, they took on the cause in part because Ms. Moss has Type 1 diabetes and has struggled on and off to stay insured, though now she has Medicaid under the Affordable Care Act’s expansion of the program. Ms. Moss, 30, went to see Ms. Finkenauer in her district office this year and asked if she supported a government system that eliminated insurance. Ms. Finkenauer, she said, stated her preference for a public option.
“That’s simply a compromise that leaves the insurance companies still in the game,” said Mr. Meier, who recently started working at John Deere building backhoes and will soon have employer-based coverage after being uninsured for his entire adult life.
The Jayapal and Sanders bills would both expand traditional Medicare to cover all Americans, and change the structure of the program to cover more services and eliminate most deductibles and co-payments. There would effectively be no private health insurance, because the new system would cover almost everything; Mr. Sanders has said private coverage could be sold for extras like cosmetic surgery.
A few houses down, a woman who owns a cleaning service and would give only her first name, Sharon, and her party affiliation, Republican, said that if the bill covered abortions, “I won’t go for that.”
She added that she would be happy to stop paying $170 a month for supplemental insurance to cover what Medicare does not, but she did not want to see people who do not work receive free care. From the garage, her husband hollered that he agreed. Conceding defeat, Mr. Meier and Ms. Moss moved along.
Both Sanders supporters, they took on the cause in part because Ms. Moss has Type 1 diabetes and has struggled on and off to stay insured, though now she has Medicaid under the Affordable Care Act’s expansion of the program. Ms. Moss, 30, went to see Ms. Finkenauer in her district office this year and asked if she supported a government system that eliminated insurance. Ms. Finkenauer, she said, stated her preference for a public option.
“That’s simply a compromise that leaves the insurance companies still in the game,” said Mr. Meier, who recently started working at John Deere building backhoes and will soon have employer-based coverage after being uninsured for his entire adult life.
The Jayapal and Sanders bills would both expand traditional Medicare to cover all Americans, and change the structure of the program to cover more services and eliminate most deductibles and co-payments. There would effectively be no private health insurance, because the new system would cover almost everything; Mr. Sanders has said private coverage could be sold for extras like cosmetic surgery.
Mr.
Meier and Ms. Moss have knocked on 250 doors and gathered about 50
signatures over the last few months. About 20 other volunteers,
including a retired nurse and several college students, are also
involved.
While polling does show
that Medicare for all has broad public support, that drops once people
learn it would involve raising taxes or eliminating private insurance.
That finding bewilders Mr. Meier, given many of the conversations he has
on people’s front steps.
Those conversations keep
coming. Rick Plowman 66, complained bitterly about how despite having
Medicare, he had to pay nearly $500 for inhalers to treat his chronic
obstructive pulmonary disease. Still, he was skeptical.
“I just don’t know what it’s going to look like down the road,” Mr. Plowman said. “Even Social Security for kids, you know? Even for you guys?”
“I’m willing to start making that sacrifice right now,” Mr. Meier pushed back. Mr. Plowman signed the petition.
At a white bungalow around the corner, Mr. Meier found — finally — that he was preaching to the choir with Bobby Daniels, 50, and his wife, Andrea, 46. Mr. Daniels, a forklift operator from Waterloo, said their coverage came with a $3,000 deductible and he would “most definitely” support Medicare for all. Ray Edwards, 36, an uninsured barber, also heartily signed on.
At the final stop of the day, Mr. Meier and Ms. Moss encountered Jeremy Shade, 36, a registered Republican who promptly told them his sister lived in Canada and had spent “hours and hours in the hospital, waiting for care” under that country’s single-payer system.
“I get that concern, and it’s something I’m worried about, too,” Mr. Meier said as Mr. Shade’s dog barked. “Would you be interested in maybe just calling Abby Finkenauer and saying, ‘Hey, what are we doing about the health care problem in this country?’”
“My wife would,” Mr. Shade said, explaining that she was a Democrat. “I’m real wary about it.”
Two hours of hot canvassing amid swarms of gnats had yielded six petition signatures and a few pledges to call Ms. Finkenauer. Mr. Meier was determined to end on a positive note. “I really think health care could be the issue that could get people to stop being so on one side or the other,” he said, a point that Mr. Shade accepted, shaking his hand before retreating inside.
https://www.nytimes.com/2019/06/15/us/politics/medicare-for-all-democrats.html?smid=nytcore-ios-share
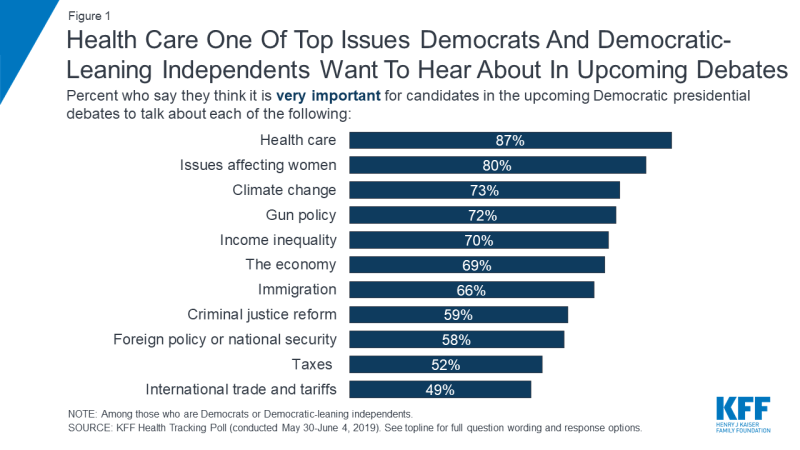
About seven in ten say it is “very important” for the candidates to
discuss climate change (73 percent), gun policy (72 percent), income
inequality (70 percent), the economy (69 percent), and immigration (66
percent). These are followed by criminal justice reform (59 percent),
foreign policy or national security (58 percent), and about half say it
is “very important” for the candidates to talk about taxes (52 percent)
and international trade and tariffs (49 percent) in the upcoming
Democratic debates.
When those who say health care is at least somewhat important for 2020 Democratic presidential candidates to discuss in upcoming debates are asked to offer in their own words what specifically about health care they want to hear about, nearly three in ten Democrats and Democratic-leaning independents overall offer responses related to lowering the amount people pay for health care (28 percent) and another eight percent explicitly mention lowering prescription drug costs. To learn more about Americans’ experiences with health care costs, check out this data note.
Access to health care also emerges as a key issue with one in five (18 percent) offering responses related to increasing access to health care and an additional 15 percent explicitly mentioning implementing a single-payer or Medicare-for-all system. The 2010 Affordable Care Act is also still on the minds of Democrats and Democratic-leaning independents with one in six mentioning protecting the Affordable Care Act and protections for people with pre-existing conditions (16 percent) as the top health care issue they want to hear about during the upcoming presidential debates. An additional one in ten (8 percent) offer access to reproductive health care services.
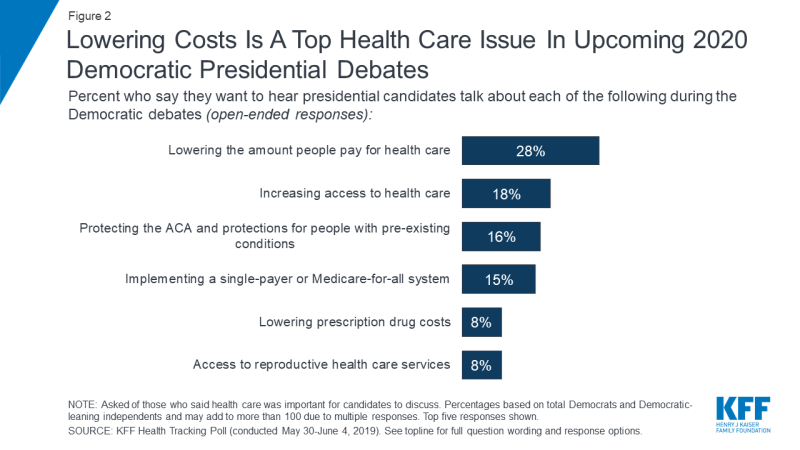
Though lowering costs and increasing access emerge as the top issues
that Democrats and Democratic-leaning independents want to hear
presidential candidates talk about, there are some notable differences
between liberals and moderates. One-fourth of liberal Democrats and
Democratic-leaning independents (23 percent) offer implementing a
single-payer or Medicare-for-all system when asked what health care
issue they want to hear the candidates discuss, making it among the top
health care issues offered by this group along with increasing access
(27 percent) and lowering the amount people pay for health care (24
percent). Among moderate Democrats and Democratic-leaning independents,
more than three times as many offer lowering the amount people pay for
health care (34 percent) than implementing a Medicare-for-all system (9
percent).
Kaiser Family Foundation Focus Groups
During the spring of 2019, Kaiser Family Foundation conducted a series of 6 focus groups with a total of 56 participants in Texas, Florida, and Pennsylvania, examining voters’ top health care issues and their views of various national health care proposals. The groups included Republicans, Democrats, independents, seniors, and young adults, and found a disconnect between what the public is talking about when it comes to health care compared to the political discussions happening in Washington, D.C. and on the 2020 campaign trail. Read Drew Altman’s takeaways from the KFF focus groups here.
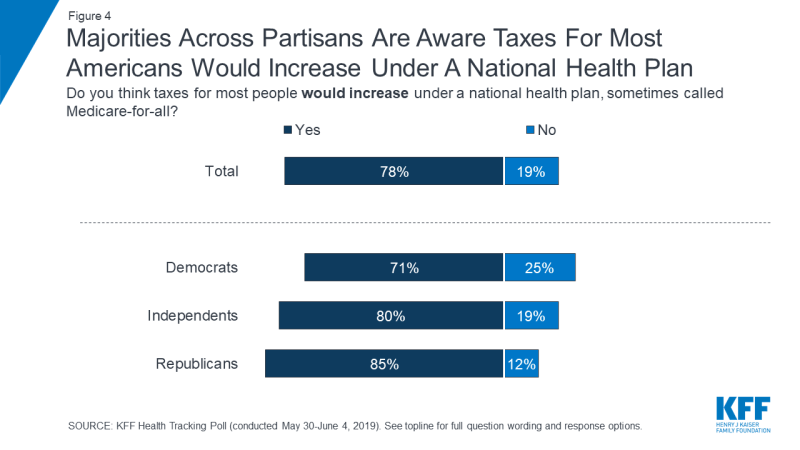
Eight in ten (78 percent) think that under a national health plan, sometimes called Medicare-for-all, taxes for most people would increase. Majorities of Democrats (71 percent), independents (80 percent), and Republicans (85 percent) say that taxes for most Americans would increase under a national health plan.
In addition, about half of Americans (53 percent) – including half of
Democrats and independents (52 percent each) and most Republicans (57
percent) – think that under a national health plan, private health
insurances would no longer be the primary way Americans would get health
coverage. Still, a substantial four in ten of the public believe that
under such a plan, private health insurance companies would still be the
primary source of coverage for most Americans and an additional seven
percent say they do not know what would happen under a national health
plan.
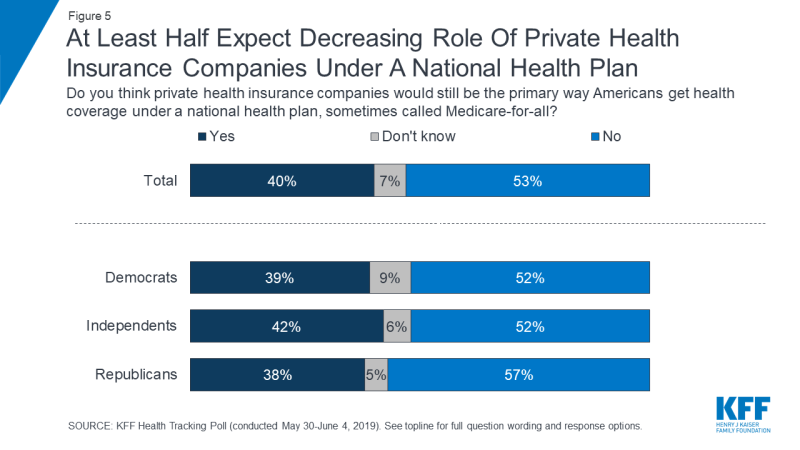
In focus groups, many participants expressed skepticism about the
idea that private insurance companies would cease to exist under a
Medicare-for-all plan. Some thought these companies were just too
powerful, and others thought they would continue to exist for people who
want to buy extra coverage beyond what a national plan would offer.
Focus group findings also indicate that many people don’t believe a
Medicare-for-all plan would result in the elimination of health
insurance premiums or cost-sharing.
Methodology
California is beefing up Obamacare, restoring an individual mandate, expanding health insurance subsidies well into the middle class and covering some undocumented adults through Medicaid. It’s an incremental step toward universal coverage that can animate the Democrats’ party-defining debate over how best to cover everyone — through a mixed public-private system or through “Medicare for All."
The Democratic-controlled state legislature on Thursday approved a budget, clearing the path for a statewide penalty for failing to purchase health insurance, which will help subsidize coverage for middle-income people earning too much to receive federal financial help from Obamacare. California will also become the first state to extend Medicaid coverage to low-income undocumented adults up to age 26, defying the Trump administration’s efforts to shrink government benefits to immigrants.
Story Continued Below
The moves fall well short of a sweeping Medicare for All-style system vigorously supported by the party’s progressive wing here in California and across the country — and viewed much more cautiously by much of the Democratic establishment.
The idea of expanding Obamacare subsidies could gain traction among more moderate Democrats in Washington who would rather build on the Affordable Care Act than engage in another protracted health reform battle should the party take back control in Washington. And they can sell it as a practical move toward expanding coverage immediately while the party weighs more progressive health plans.
“I view California as a model state that’s likely to be used as a best practices example for how Congress can move ahead in a new Democratic administration without in any way creating barriers to do more aggressive policies in the future,” said Chris Jennings, who was a health policy adviser in the Clinton and Obama administrations.
Case in point: California’s new progressive governor, Gavin Newsom, said he remains committed to setting up a single-payer system in the state, but he made the Obamacare expansion and coverage for undocumented immigrants a priority his first year.
Peter Lee, executive director of Covered California, the state's Obamacare marketplace, said the legislature’s coverage expansion was an indication “we can’t stand still” while others debate more sweeping overhauls of the health care system.
California's plan isn’t a done deal. Having cleared the $215 billion budget, state lawmakers in the coming days must pass a series of bills approving the health measures through an expedited process.
House Democratic leaders in Washington, wary of a pursuing a fully government-run single-payer system, have embraced a key element of the California plan. They unveiled a package this spring that would vastly expand eligibility for health insurance subsidies, though it didn't include reviving Obamacare's requirement to purchase coverage.
The proposed California mandate largely mirrors the federal penalty that was eliminated by Congress in late 2017. But California's mandate would be pegged to the state's income tax filing threshold, which is higher than the federal level, meaning more people would be exempt from the penalty.
The mandate penalty, along with $450 million from the state's general fund over the next three years, helps pay for the expanded subsidies. The penalty is expected to generate an estimated $295 million this coming fiscal year, and as much as $380 million in 2022.
Under Obamacare, health insurance subsidies are cut off for people earning above four times the federal poverty level, or about $50,000 for an individual. California is extending subsidies to those earning six times the poverty level, or about $75,000 for an individual. About 190,000 Californians would be eligible for those expanded subsidies.
Even if the individual mandate is eventually approved as expected, some observers say it could face challenges in the courts — and possibly come at a political price. Opponents of the idea have criticized California for restoring the unpopular individual mandate while also extending Medicaid coverage to about 90,000 undocumented immigrants.
Story Continued Below
“How, for Pete’s sake, do you impose an individual mandate on contributing taxpayers who are citizens of California and subsidize undocumented immigrants by giving them free health care?” said Jon Coupal, president of the Howard Jarvis Taxpayers Association in California. “There’s an equity issue here that’s going to be part of the political miss.”
California is covering most of the cost of Medicaid coverage for young undocumented adults, estimated at $98 million this year. Still, the state is planning to draw some federal funds for this group, which could spark pushback from the Trump administration.
Coupal said the way the Legislature is advancing the mandate makes it ripe for a legal challenge. He said it amounts to a new tax, meaning it should go through regular legislative order instead of the fast-track budget process.
David McCuan, a California political analyst, said the state's health proposals "mark California as a barometer of where health care can go,” but he also expects to see “numerous” legal challenges, particularly over the mandate.
Several health experts pointed out that a handful of states have passed individual mandates since Congress gutted Obamacare's — including New Jersey, Vermont and Washington, D.C — and none have been challenged in court. Rhode Island lawmakers are also considering mandate legislation this year. Massachusetts was the first state to pass an individual mandate in 2006, and it became the model for the Affordable Care Act.
https://www.politico.com/story/2019/06/16/california-obamacare-health-care-1530461?
“I just don’t know what it’s going to look like down the road,” Mr. Plowman said. “Even Social Security for kids, you know? Even for you guys?”
“I’m willing to start making that sacrifice right now,” Mr. Meier pushed back. Mr. Plowman signed the petition.
At a white bungalow around the corner, Mr. Meier found — finally — that he was preaching to the choir with Bobby Daniels, 50, and his wife, Andrea, 46. Mr. Daniels, a forklift operator from Waterloo, said their coverage came with a $3,000 deductible and he would “most definitely” support Medicare for all. Ray Edwards, 36, an uninsured barber, also heartily signed on.
At the final stop of the day, Mr. Meier and Ms. Moss encountered Jeremy Shade, 36, a registered Republican who promptly told them his sister lived in Canada and had spent “hours and hours in the hospital, waiting for care” under that country’s single-payer system.
“I get that concern, and it’s something I’m worried about, too,” Mr. Meier said as Mr. Shade’s dog barked. “Would you be interested in maybe just calling Abby Finkenauer and saying, ‘Hey, what are we doing about the health care problem in this country?’”
“My wife would,” Mr. Shade said, explaining that she was a Democrat. “I’m real wary about it.”
Two hours of hot canvassing amid swarms of gnats had yielded six petition signatures and a few pledges to call Ms. Finkenauer. Mr. Meier was determined to end on a positive note. “I really think health care could be the issue that could get people to stop being so on one side or the other,” he said, a point that Mr. Shade accepted, shaking his hand before retreating inside.
https://www.nytimes.com/2019/06/15/us/politics/medicare-for-all-democrats.html?smid=nytcore-ios-share
KFF Health Tracking Poll – June 2019: Health Care in the Democratic Primary and Medicare-for-all - Findings
Kaiser Family Foundation - June 2019
Key Findings:
- Health care is leading the list of possible topics Democrats and Democratic-leaning independents want to hear the 2020 Democratic presidential candidates talk about during their upcoming debates, with nearly nine in ten (87 percent) saying it is very important for candidates to talk about health care. This is closely followed by eight in ten who say it is very important for candidates to discuss issues affecting women, perhaps reflecting recent news attention on these issues. Health care and women’s issues rank ahead of other top issues for Democrats and Democratic-leaning independents such as climate change (73 percent), gun policy (72 percent), income inequality (70 percent), the economy (69 percent), and immigration (66 percent).
- When asked to say in their own words which health care issues they
want to hear candidates discuss, affordability emerges as a top issue
with nearly three in ten Democrats and Democratic-leaning independents
mentioning lowering the amount people pay for health care (28 percent). A further eight percent mention lowering the cost of prescription drugs. Access to health care also emerges as a key topic with one in five mentioning increasing access to health care (18 percent) while an additional 15 percent explicitly mention implementing a single-payer or Medicare-for-all system.
Poll: Most Americans don’t realize how dramatically the leading Medicare-for-all proposals would restructure the nation’s health care system
- The most recent KFF Health Tracking Poll finds majorities across partisans think taxes for most people would increase under a national health plan, sometimes called Medicare-for-all (78 percent), and about half (53 percent) think private health insurance companies would no longer be the primary way Americans would get health coverage under such a plan. However, when it comes to other key changes that the leading Medicare-for-all bills introduced by Sen. Bernie Sanders and Rep. Pramila Jayapal would bring, large shares are unaware of how the current health care system may be affected. For example, majorities say people would continue to pay deductibles and co-pays (69 percent) and continue to pay premiums (54 percent) under a Medicare-for-all plan. Likewise, majorities say people with employer-sponsored or self-purchased insurance would be able to keep their plans (55 percent each) under a Medicare-for-all plan.
- Overall, nearly half of the public (46 percent) hold favorable views of the 2010 Affordable Care Act while four in ten hold unfavorable views. Majorities of Democrats continue to hold favorable views towards the law while majorities of Republicans hold unfavorable views. Independents are more divided with similar shares holding favorable and unfavorable views. To see the shifts in public attitudes towards the law over time, check out the KFF interactive.
Health Care in The Democratic Primary
What do Democrats want their 2020 presidential candidates to talk about heading into the primary debates? Health care and issues affecting women top their priority list in this @KaiserFamFound pollLess than one month before the first 2020 Democratic presidential primary debate, KFF polling finds health care is among the top issues that Democrats and Democratic-leaning independents want to hear the candidates talk about during the upcoming debates. Nearly nine in ten Democrats and Democratic-leaning independents (87 percent) say it is “very important” for the candidates to talk about health care during the upcoming Democratic presidential debates. This is followed by eight in ten who say it is “very important” for the candidates to discuss issues that affect women, an issue that garnered recent media attention.
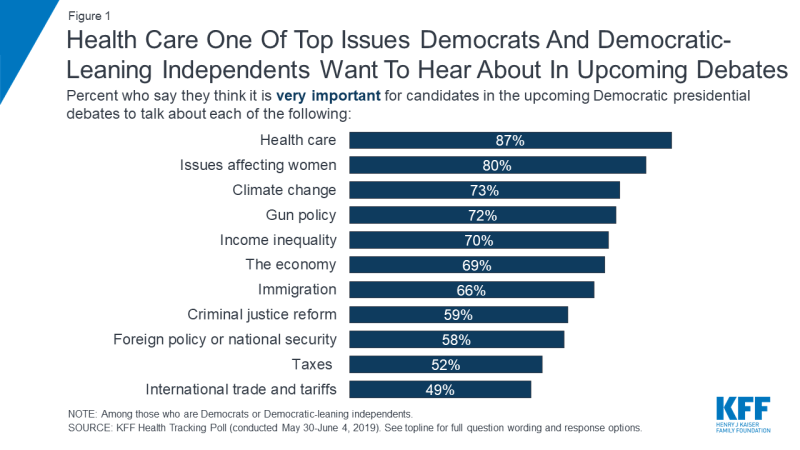
Figure 1: Health Care One Of Top Issues Democrats And Democratic-Leaning Independents Want To Hear About In Upcoming Debates
When those who say health care is at least somewhat important for 2020 Democratic presidential candidates to discuss in upcoming debates are asked to offer in their own words what specifically about health care they want to hear about, nearly three in ten Democrats and Democratic-leaning independents overall offer responses related to lowering the amount people pay for health care (28 percent) and another eight percent explicitly mention lowering prescription drug costs. To learn more about Americans’ experiences with health care costs, check out this data note.
Access to health care also emerges as a key issue with one in five (18 percent) offering responses related to increasing access to health care and an additional 15 percent explicitly mentioning implementing a single-payer or Medicare-for-all system. The 2010 Affordable Care Act is also still on the minds of Democrats and Democratic-leaning independents with one in six mentioning protecting the Affordable Care Act and protections for people with pre-existing conditions (16 percent) as the top health care issue they want to hear about during the upcoming presidential debates. An additional one in ten (8 percent) offer access to reproductive health care services.
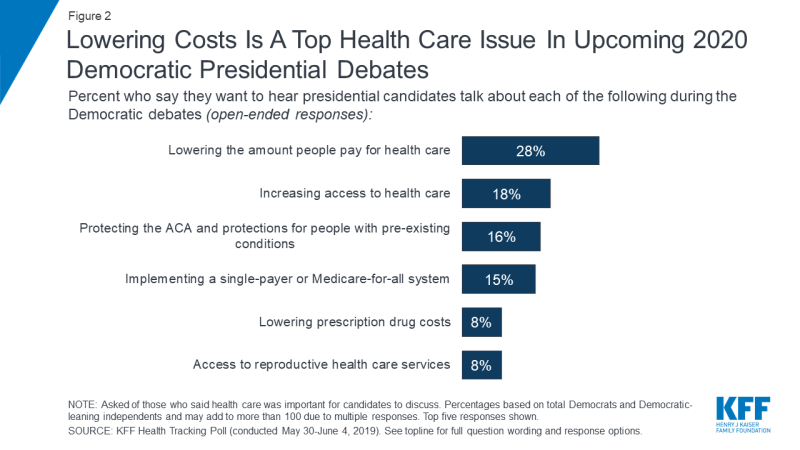
Figure 2: Lowering Costs Is A Top Health Care Issue In Upcoming 2020 Democratic Presidential Debates
Kaiser Family Foundation Focus Groups
During the spring of 2019, Kaiser Family Foundation conducted a series of 6 focus groups with a total of 56 participants in Texas, Florida, and Pennsylvania, examining voters’ top health care issues and their views of various national health care proposals. The groups included Republicans, Democrats, independents, seniors, and young adults, and found a disconnect between what the public is talking about when it comes to health care compared to the political discussions happening in Washington, D.C. and on the 2020 campaign trail. Read Drew Altman’s takeaways from the KFF focus groups here.
A National Health Plan or Medicare-for-all
Implementing a national health plan, sometimes called Medicare-for-all, has been a dominant issue during the 2020 Democratic primary. Previous KFF polling has found that a slight majority supports the idea of a national health plan, but attitudes towards such a proposal are fairly malleable with significant shares, on either side of the debate, shifting their opinion once they hear counter-arguments. With several bills being introduced in the 116th Congress that would expand the role of public programs in health, this month’s Kaiser Health Tracking Poll examines the public’s awareness on key aspects of Medicare-for-all plans including Sen. Sanders’ Medicare for All Act of 2019 and Rep. Japayal’s bill of the same name.1Eight in ten (78 percent) think that under a national health plan, sometimes called Medicare-for-all, taxes for most people would increase. Majorities of Democrats (71 percent), independents (80 percent), and Republicans (85 percent) say that taxes for most Americans would increase under a national health plan.
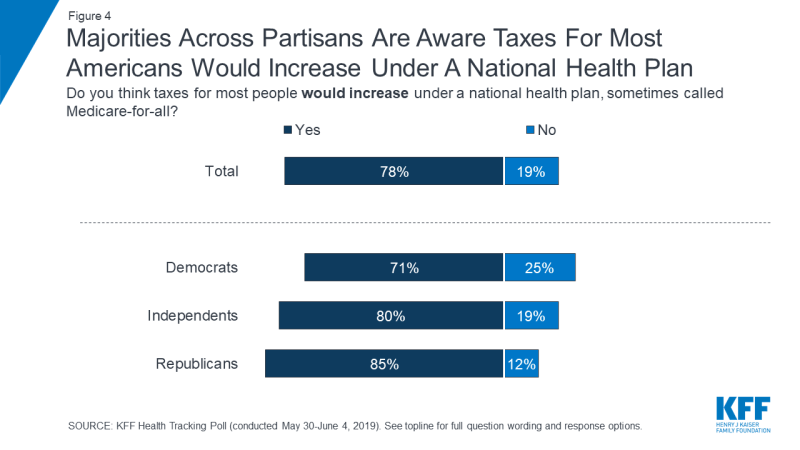
Figure 4: Majorities Across Partisans Are Aware Taxes For Most Americans Would Increase Under A National Health Plan
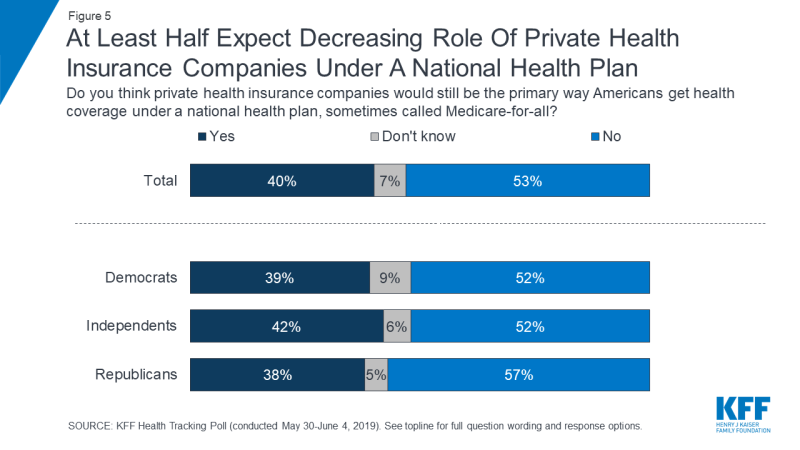
Figure 5: At Least Half Expect Decreasing Role Of Private Health Insurance Companies Under A National Health Plan
In their own words: Focus group participants on private insurance
[Moderator: Do you think Medicare-for-all means that private health insurance companies will go away?]
“No, because they’d be running Medicare-for-all.” (Houston, independent)
“Or even those individuals who can afford to have the type of coverage they want, they wouldn’t want a basic burger. No, they want to add all of the extra fixings because they can afford it.” (Houston, independent)
“They’re going to take a hit obviously but I don’t think that they’re really going to go away. They’re too powerful.” (Harrisburg, Democrat)
“I don’t think for a second that private insurance would go away, even if you implemented this. There will always be the Cadillac plan that is available, because as long as somebody—the market will react.” (Orlando, Democrat)
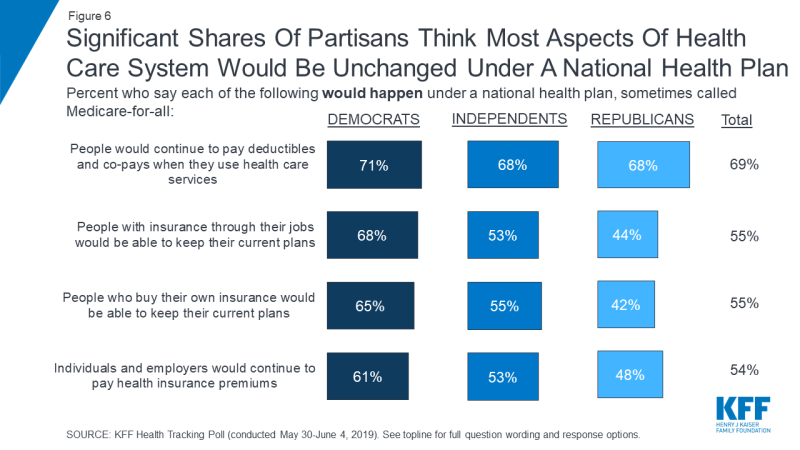
When it comes to other potential impacts of a national health plan,
many Americans say most aspects of the current health care system would
remain unchanged. Majorities of Democrats, independents, and Republicans
say people would continue to pay deductibles and co-pays when they use
health care services (71 percent, 68 percent, and 68 percent,
respectively). In addition, majorities of both Democrats and
independents also believe people with employer-sponsored insurance would
be able to keep their current coverage (68 percent and 53 percent),
people who purchase their own plans would be able to keep their current
coverage (65 percent and 55 percent), and individuals and employers
would continue to pay health insurance premiums (61 percent and 53
percent). At least four in ten Republicans also say each of these things
would happen under a national health plan. Small shares of the public
overall say they don’t know whether each of these things would happen
under such a plan (4 percent say they don’t know if people would
continue to pay deductibles and co-pays, 7 percent say they don’t know
for the other changes included).[Moderator: Do you think Medicare-for-all means that private health insurance companies will go away?]
“No, because they’d be running Medicare-for-all.” (Houston, independent)
“Or even those individuals who can afford to have the type of coverage they want, they wouldn’t want a basic burger. No, they want to add all of the extra fixings because they can afford it.” (Houston, independent)
“They’re going to take a hit obviously but I don’t think that they’re really going to go away. They’re too powerful.” (Harrisburg, Democrat)
“I don’t think for a second that private insurance would go away, even if you implemented this. There will always be the Cadillac plan that is available, because as long as somebody—the market will react.” (Orlando, Democrat)
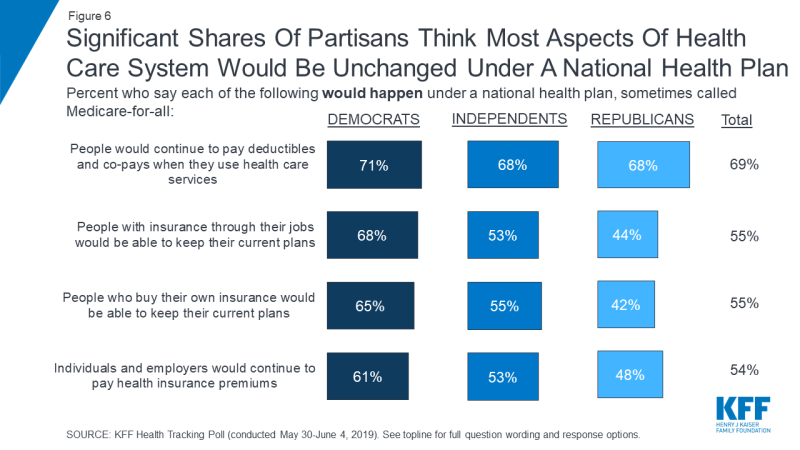
Figure
6: Significant Shares Of Partisans Think Most Aspects Of Health Care
System Would Be Unchanged Under A National Health Plan
In their own words: Focus group participants on premiums and cost-sharing
[Moderator: Do you think Medicare-for-all means that there would be no more co-pays or deductibles when people use care?]
“No, I think there’d probably still be co-pays and deductibles, but just be affordable.” (Houston, independent)
“It wouldn’t make sense to you that you wouldn’t have to pay [co-pays and deductibles] because it wouldn’t feel sustainable.” (Houston, independent)
“My mom is on Medicare and she has to pay co-pays.” (Houston, independent)
There is a partisan divide on some aspects of how a national health
plan would affect people and health care providers. Three-fourths of
Democrats (76 percent) say that all U.S. residents would have health
insurance coverage under a national health plan while about half of
Republicans say this would not happen (49 percent). On
the other hand, most Republicans say a national health plan would lead
to doctors and hospitals being paid less (64 percent) while about half
of Democrats say this would not happen (48 percent).
Large shares of independents believe both of these things would happen,
with six in ten (61 percent) saying all U.S. residents would get health
coverage and half saying doctors and hospitals would be paid less.[Moderator: Do you think Medicare-for-all means that there would be no more co-pays or deductibles when people use care?]
“No, I think there’d probably still be co-pays and deductibles, but just be affordable.” (Houston, independent)
“It wouldn’t make sense to you that you wouldn’t have to pay [co-pays and deductibles] because it wouldn’t feel sustainable.” (Houston, independent)
“My mom is on Medicare and she has to pay co-pays.” (Houston, independent)
| Table 1: Partisans Disagree On Some Basic Implications of a National Health Plan | ||||
| Percent who think each of the following would happen under a national plan, sometimes called Medicare-for-all: | Total | Democrats | Independents | Republicans |
| Taxes for most people would increase | 78% | 71% | 80% | 85% |
| All U.S. residents would have health insurance coverage | 62 | 76 | 61 | 45 |
| Private health insurance companies would NOT be the primary way Americans get health coverage | 53 | 52 | 52 | 57 |
| Doctors and hospitals would be paid less | 52 | 42 | 50 | 64 |
| People who buy their own insurance would NOT be able to keep their current plans | 39 | 24 | 40 | 53 |
| Individuals and employers would NOT continue to pay health insurance premiums | 39 | 31 | 42 | 45 |
| People with employer-sponsored insurance would NOT be able to keep their current plans | 38 | 25 | 42 | 47 |
| People would NOT continue to pay deductibles and co-pays when they use health care services | 27 | 25 | 29 | 28 |
Public Views of The ACA
While the public still holds largely partisan views over the Affordable Care Act and opinions have remained relatively unchanged for the past two years since the Republican efforts to repeal the law, views are down slightly this month. Nearly half of the public (46 percent) hold favorable opinions of the ACA while four in ten hold a negative opinion of the law. Across partisans, nearly eight in ten Democrats (79 percent) have a favorable view of the ACA compared to nearly half of independents (47 percent), and about one-sixth of Republicans (16 percent).Methodology
California goes even bigger on Obamacare
by Victoria Colliver - Politico - June 18, 20190
The state is advancing a sweeping health care package that could shape Democrats' debate over universal coverage.California is beefing up Obamacare, restoring an individual mandate, expanding health insurance subsidies well into the middle class and covering some undocumented adults through Medicaid. It’s an incremental step toward universal coverage that can animate the Democrats’ party-defining debate over how best to cover everyone — through a mixed public-private system or through “Medicare for All."
The Democratic-controlled state legislature on Thursday approved a budget, clearing the path for a statewide penalty for failing to purchase health insurance, which will help subsidize coverage for middle-income people earning too much to receive federal financial help from Obamacare. California will also become the first state to extend Medicaid coverage to low-income undocumented adults up to age 26, defying the Trump administration’s efforts to shrink government benefits to immigrants.
Story Continued Below
The moves fall well short of a sweeping Medicare for All-style system vigorously supported by the party’s progressive wing here in California and across the country — and viewed much more cautiously by much of the Democratic establishment.
The idea of expanding Obamacare subsidies could gain traction among more moderate Democrats in Washington who would rather build on the Affordable Care Act than engage in another protracted health reform battle should the party take back control in Washington. And they can sell it as a practical move toward expanding coverage immediately while the party weighs more progressive health plans.
“I view California as a model state that’s likely to be used as a best practices example for how Congress can move ahead in a new Democratic administration without in any way creating barriers to do more aggressive policies in the future,” said Chris Jennings, who was a health policy adviser in the Clinton and Obama administrations.
Case in point: California’s new progressive governor, Gavin Newsom, said he remains committed to setting up a single-payer system in the state, but he made the Obamacare expansion and coverage for undocumented immigrants a priority his first year.
Peter Lee, executive director of Covered California, the state's Obamacare marketplace, said the legislature’s coverage expansion was an indication “we can’t stand still” while others debate more sweeping overhauls of the health care system.
California's plan isn’t a done deal. Having cleared the $215 billion budget, state lawmakers in the coming days must pass a series of bills approving the health measures through an expedited process.
House Democratic leaders in Washington, wary of a pursuing a fully government-run single-payer system, have embraced a key element of the California plan. They unveiled a package this spring that would vastly expand eligibility for health insurance subsidies, though it didn't include reviving Obamacare's requirement to purchase coverage.
The proposed California mandate largely mirrors the federal penalty that was eliminated by Congress in late 2017. But California's mandate would be pegged to the state's income tax filing threshold, which is higher than the federal level, meaning more people would be exempt from the penalty.
The mandate penalty, along with $450 million from the state's general fund over the next three years, helps pay for the expanded subsidies. The penalty is expected to generate an estimated $295 million this coming fiscal year, and as much as $380 million in 2022.
Under Obamacare, health insurance subsidies are cut off for people earning above four times the federal poverty level, or about $50,000 for an individual. California is extending subsidies to those earning six times the poverty level, or about $75,000 for an individual. About 190,000 Californians would be eligible for those expanded subsidies.
Even if the individual mandate is eventually approved as expected, some observers say it could face challenges in the courts — and possibly come at a political price. Opponents of the idea have criticized California for restoring the unpopular individual mandate while also extending Medicaid coverage to about 90,000 undocumented immigrants.
Story Continued Below
“How, for Pete’s sake, do you impose an individual mandate on contributing taxpayers who are citizens of California and subsidize undocumented immigrants by giving them free health care?” said Jon Coupal, president of the Howard Jarvis Taxpayers Association in California. “There’s an equity issue here that’s going to be part of the political miss.”
California is covering most of the cost of Medicaid coverage for young undocumented adults, estimated at $98 million this year. Still, the state is planning to draw some federal funds for this group, which could spark pushback from the Trump administration.
Coupal said the way the Legislature is advancing the mandate makes it ripe for a legal challenge. He said it amounts to a new tax, meaning it should go through regular legislative order instead of the fast-track budget process.
David McCuan, a California political analyst, said the state's health proposals "mark California as a barometer of where health care can go,” but he also expects to see “numerous” legal challenges, particularly over the mandate.
Several health experts pointed out that a handful of states have passed individual mandates since Congress gutted Obamacare's — including New Jersey, Vermont and Washington, D.C — and none have been challenged in court. Rhode Island lawmakers are also considering mandate legislation this year. Massachusetts was the first state to pass an individual mandate in 2006, and it became the model for the Affordable Care Act.
https://www.politico.com/story/2019/06/16/california-obamacare-health-care-1530461?
Florida Company Sued Over Sales of Skimpy Health Plans
by Reed Abelson - NYT - June 12, 2019
One Ohio
resident paid $240 a month for health insurance that she later learned
didn’t cover her knee replacement. Saddled with $48,000 in medical
bills, she decided not to get the other knee replaced.
“It’s been devastating to me,” said Elizabeth Belin, who lives in Columbus. The bills totaled more than her annual salary.
A Kansas resident paid premiums on a policy for two years, then found out his insurance would not cover surgery for a newly diagnosed cancer.
The two policyholders have filed a lawsuit in federal court against Health Insurance Innovations, based in Tampa, Fla., accusing the company of misleading them about the kind of policy they were buying.
“It’s been devastating to me,” said Elizabeth Belin, who lives in Columbus. The bills totaled more than her annual salary.
A Kansas resident paid premiums on a policy for two years, then found out his insurance would not cover surgery for a newly diagnosed cancer.
The two policyholders have filed a lawsuit in federal court against Health Insurance Innovations, based in Tampa, Fla., accusing the company of misleading them about the kind of policy they were buying.
They
say they believed they were purchasing Affordable Care Act plans that
include coverage guarantees. But they were sold much less comprehensive
coverage that left them vulnerable to tens of thousands of dollars in
unpaid medical bills, according to the lawsuit.
Their complaints underscore problems with some types of cheaper health insurance alternatives that the Trump administration has expanded. Critics of the government’s decision, including the Association for Community Affiliated Plans and the National Alliance on Mental Illness, are also suing the Trump administration over relaxation of rules for these plans.
“This isn’t real insurance,” said Jason Kellogg, one of the lawyers representing the individuals in the Florida case. They are seeking class-action status, estimating that as many as 500,000 people may have bought these policies.
In an emailed statement, Health Insurance Innovations said the lawsuit was without merit. “We will vigorously defend ourselves against all such allegations,” the company said.
Proponents of short-term plans say they represent an affordable option for those who can’t pay for the robust coverage mandated by the federal law.
Their complaints underscore problems with some types of cheaper health insurance alternatives that the Trump administration has expanded. Critics of the government’s decision, including the Association for Community Affiliated Plans and the National Alliance on Mental Illness, are also suing the Trump administration over relaxation of rules for these plans.
“This isn’t real insurance,” said Jason Kellogg, one of the lawyers representing the individuals in the Florida case. They are seeking class-action status, estimating that as many as 500,000 people may have bought these policies.
In an emailed statement, Health Insurance Innovations said the lawsuit was without merit. “We will vigorously defend ourselves against all such allegations,” the company said.
Proponents of short-term plans say they represent an affordable option for those who can’t pay for the robust coverage mandated by the federal law.
But a recent report
by researchers from the Georgetown University Center on Health
Insurance Reforms concluded that the lack of oversight meant that
“consumers are at risk of being underinsured, with significant financial
liability if a high-cost medical event occurs.”
Four states — California, Massachusetts, New Jersey and New York — have largely banned the sale of these products, and others have restricted sales of such plans, according to another analysis.
Jessica Altman, the insurance commissioner for Pennsylvania, told lawmakers at a congressional hearing this year that the state had taken action against eight companies in the last two years for misrepresenting the kind of coverage being sold.
In recent months, Congress has become increasingly concerned about consumers burdened by medical debt, putting a spotlight on surprise medical bills.
At the news conference on Wednesday, Ms. Belin and Christopher Mitchell, the plaintiffs in the lawsuit, said they had no idea they were buying junk insurance.
Ms. Belin, who was recently divorced, had been looking for an Obamacare policy in 2016. She spoke to a sales agent who offered her what she thought was an array of traditional health plans.
“He would find me a plan that would fit my budget,” she recalled being told. Instead, she was sold a limited benefit plan, which sharply capped what it paid for medical care.
Four states — California, Massachusetts, New Jersey and New York — have largely banned the sale of these products, and others have restricted sales of such plans, according to another analysis.
Jessica Altman, the insurance commissioner for Pennsylvania, told lawmakers at a congressional hearing this year that the state had taken action against eight companies in the last two years for misrepresenting the kind of coverage being sold.
In recent months, Congress has become increasingly concerned about consumers burdened by medical debt, putting a spotlight on surprise medical bills.
At the news conference on Wednesday, Ms. Belin and Christopher Mitchell, the plaintiffs in the lawsuit, said they had no idea they were buying junk insurance.
Ms. Belin, who was recently divorced, had been looking for an Obamacare policy in 2016. She spoke to a sales agent who offered her what she thought was an array of traditional health plans.
“He would find me a plan that would fit my budget,” she recalled being told. Instead, she was sold a limited benefit plan, which sharply capped what it paid for medical care.
Mr.
Mitchell bought a similar policy the same year from a broker who
promised to find the best plan in Kansas at the best price. He was found
to have invasive ductal carcinoma, a type of breast cancer, in early
2018. His doctor told him that he needed surgery, but the hospital where
it was scheduled told him that he did not have insurance coverage.
According to the complaint, Health Insurance Innovations participated in a scheme involving Simple Health, another Florida company, whose agents sold them the flimsy coverage. Simple Health was recently shut down by the Federal Trade Commission after regulators accused it of being “a classic bait and switch scheme,” according to court filings.
The lawsuit claims Health Insurance Innovations spent millions of dollars funding Simple Health and was intimately involved in the scripts its brokers used to sell these policies. Customers were told that they were getting a P.P.O. plan, a traditional policy that allows individuals to go to the doctor or hospital of their choice. Many of the websites that consumers visited implied the policies being offered were from brand-name insurers.
The lawsuit quotes from the scripts being used by the brokers. “What’s the point of paying all that money every month if it’s not going to cover the most important things, right???” the broker asks. “This plan covers you from Day 1 …’”
Health Insurance Innovations says it was never involved in Simple Health’s activities. While the company said it had relied on Simple Health brokers to sell policies and collected the premium payments, it required all brokers “to provide clear disclosure of the information necessary for consumers to understand the policies they purchase,” according to its statement.
“Simple Health violated the trust of its consumers, its regulators and us,” the company said, emphasizing that it was not named as a defendant in the F.T.C. case and was cooperating with federal regulators.
The company said it cut its ties to Simple Health last year after the F.T.C. took action against the company.
According to the complaint, Health Insurance Innovations participated in a scheme involving Simple Health, another Florida company, whose agents sold them the flimsy coverage. Simple Health was recently shut down by the Federal Trade Commission after regulators accused it of being “a classic bait and switch scheme,” according to court filings.
The lawsuit claims Health Insurance Innovations spent millions of dollars funding Simple Health and was intimately involved in the scripts its brokers used to sell these policies. Customers were told that they were getting a P.P.O. plan, a traditional policy that allows individuals to go to the doctor or hospital of their choice. Many of the websites that consumers visited implied the policies being offered were from brand-name insurers.
The lawsuit quotes from the scripts being used by the brokers. “What’s the point of paying all that money every month if it’s not going to cover the most important things, right???” the broker asks. “This plan covers you from Day 1 …’”
Health Insurance Innovations says it was never involved in Simple Health’s activities. While the company said it had relied on Simple Health brokers to sell policies and collected the premium payments, it required all brokers “to provide clear disclosure of the information necessary for consumers to understand the policies they purchase,” according to its statement.
“Simple Health violated the trust of its consumers, its regulators and us,” the company said, emphasizing that it was not named as a defendant in the F.T.C. case and was cooperating with federal regulators.
The company said it cut its ties to Simple Health last year after the F.T.C. took action against the company.
Health
Insurance Innovations, which is publicly held, has also been embroiled
in controversy with state regulators over the sale of short-term plans.
Last December, it reached a settlement with state regulators over its marketing practices. The company denied any wrongdoing.
With a reported $352 million in sales last year, Health Insurance Innovations specializes in online sales of policies and has benefited from moves by the Trump administration to allow people greater access to plans that do not meet the Obamacare requirements.
But Mr. Mitchell says his experience should serve as a cautionary tale to those shopping for their own policies. “This could happen to anyone,” he said. “People need to be aware of these scams.”
https://www.nytimes.com/2019/06/12/health/insurance-lawsuit-obamacare.html?smid=nytcore-ios-share
With a reported $352 million in sales last year, Health Insurance Innovations specializes in online sales of policies and has benefited from moves by the Trump administration to allow people greater access to plans that do not meet the Obamacare requirements.
But Mr. Mitchell says his experience should serve as a cautionary tale to those shopping for their own policies. “This could happen to anyone,” he said. “People need to be aware of these scams.”
https://www.nytimes.com/2019/06/12/health/insurance-lawsuit-obamacare.html?smid=nytcore-ios-share
How red-baiting in medicine did lasting harm to Americans’ health care
by Merlin Chowkwanyun - Washington Post - June 12, 2019
The battle for universal health care has come a long way. Today, the House Ways and Means Committee is holding a hearing on Medicare-for-all, and the plan has recently gained support from high-ranking Democrats, including several presidential contenders. It’s traction that would have been unimaginable even a decade ago.
Even
so, the fight for Medicare-for-all will be a war. “You should not be
the guinea pigs in some far-left social experiment,” Senate Majority
Leader Mitch McConnell (R-Ky.) recently opined. These remarks echo the
pitched battle over the Affordable Care Act a decade ago and the famous ads
that helped bring down President Bill Clinton’s health-care plan,
featuring the fictitious couple Harry and Louise, who fanned fears of
limited doctor choice by remarking, “They choose. We lose.”
But
the opposition to national health insurance extends far beyond fighting
against the policy itself. Its roots are in the McCarthy period of the
1950s, when the medical profession purged from its ranks those doctors
with any hint of leftist political orientation, removing critical voices
of dissent from the mainstream health policy conversation.
In
the half-century since, the profession and its lobbyists have
frequently fought against expanded government financing of health care
for all. And they have effectively ingrained those critiques into the
larger political dialogue, making any kind of debate about health care
about not just medicine, but also fundamental faith in government and
the welfare state. Until we understand this legacy, we won’t be able to
transcend it and have a sober dialogue about the future of health care
in the United States.
In 1950, the Journal of
the American Medical Association (JAMA) published an editorial by FBI
Director J. Edgar Hoover warning about metaphorical “communist germs”
and urging physicians to forward “any information of this nature” to the
bureau.
Hoover’s editorial wasn’t just some
oddity. As the Cold War alignment hardened, the medical establishment
vigorously policed its own ranks for any hint of “red” leanings, which
meant working closely with the most repressive elements of the
government, including the FBI. In this climate, support for left-leaning
public policies put doctors’ livelihoods at risk.
In
1951, during a hearing on the motion picture industry, the House
Un-American Activities Committee (HUAC) called Los Angeles physician
Murray Abowitz to testify about his association with a group called the
National Council of Arts, Sciences and Professions (CASP), which HUAC
had concluded was “anti-American, pro-Soviet.” HUAC asked Abowitz about
other activities, too, including his work with the Civil Rights
Congress, a racial justice organization made up heavily, though not
exclusively, of Communist Party members.
After
the hearings, Abowitz promptly lost his job at Cedars of Lebanon
Hospital in Los Angeles (now merged and known as Cedars-Sinai). So did
two other doctors, Alexander Pennes and Richard Lippman, an eminent
expert on kidney disease, whose names came up in Abowitz’s testimony.
What
cost these doctors their jobs? Throwing themselves into progressive
causes. That included fighting for national health insurance, higher
wages for interns and residents, and an end to racism in hospitals.
Lippman had recently helped research a pamphlet that documented patterns
of exclusion in Los Angeles facilities, and it didn’t hold back on
identifying offending facilities by name. But embracing civil rights so
visibly was professionally dangerous, particularly in an era when the
American left and the Communist Party were major engines of civil rights
agitation.
The 1951 hearing was just the
start. A few months later, in January 1952, HUAC returned, broadening
its scope to examine “Communist Activities Among Professional Groups in
the Los Angeles Area.” An osteopath named Louise Light named names.
Soon, Harold Koppelman, a surgeon at Queen of Angels Hospital, received a
subpoena from HUAC. It cost him his job. Four additional physicians at
Cedars suffered the same fate when they, too, received HUAC summonses.
These firings
were the result of an elaborate red-baiting operation constructed by
the medical profession, working with government organs such as HUAC and
the FBI. In 1952, an FBI agent reported receiving a call from a Cedars
trustee who asked him for any information that would help in
“establishing” Lippman’s subversive activities.
Two
years later, when a state-level analogue to HUAC held hearings on
communist infiltration into the medical ranks, it did so at the behest
of the Los Angeles County Medical Association (LACMA). During the
hearings, it became clear that LACMA’s leaders had been tracking the
activities of left-wing Los Angeles physicians for some time. They had
monitored protests against the Cedars firings, even attending some
events.
Efforts to remove any “red” presence
didn’t just involve ferreting out doctors with any hint of leftist
political ties or activism. The profession also attacked groups. Into
the late 1940s, the Association of Internes and Medical Students (AIMS)
was a large activist organization that fought for better working
conditions for young physicians, built alliances with like-minded
medical students around the world and supported civil rights and
national health insurance.
This activism
brought it into the crosshairs of the powerful American Medical
Association, then at the height of a crusade against government-funded
insurance.
The AMA acted swiftly. It opened an
investigation of AIMS, writing in JAMA, one of the most influential
publications in American medicine, that the organization was “exhibiting
communistic tendencies.” A year later, another JAMA commentary
criticized AIMS’s support for national health insurance and higher wages
and drew on these earlier accusations of communist affiliations to
undermine its credibility. It ominously warned that students who joined
AIMS might “risk considerable embarrassment.”
The
AMA campaign culminated in a report concluding that AIMS regularly
published those “affiliated with organizations and institutions that
have been cited as Communist fronts” and that it had “a general
reputation of being a left wing organization.” The AMA could not, it
concluded, “lend its support” to AIMS.
AIMS’s
stigmatization had immediate consequences. At an individual level, it
cost Sheppard Thierman, an intern at Kings County Hospital, his job.
Advertisers withdrew from AIMS’s publication, starving it of its main
revenue source. Issues grew scarcer, then thinner, then nonexistent.
AIMS chapters withered away.
These episodes —
and many others like them — explain why the medical profession has been
so averse to national health insurance until very recently. Not only did
doctors risk stigma if they supported it in the 1950s, but many on the
left also had their careers derailed, skewing the profession’s political
complexion.
While doctors’ politics, and accordingly, attitudes toward national health insurance, are starting to shift,
the toxic residue of these purges remain. The silencing of progressive
physicians during the Cold War has long narrowed the horizons of what
was possible in health care. Our health-care system is worse for it,
clearly not serving all Americans well. The profession must grapple with
its legacy of political repression and how it has shaped American
health care, and then reevaluate what policies might lead to better care
for all.
Why Air Ambulance Bills Are Still Sky-High
by Rachel Bluth - Kaiser Health News - June 14, 2019
In April 2018, 9-year-old Christian Bolling was hiking with his parents and sister in Virginia's Blue Ridge Mountains, near their home in Roanoke. While climbing some boulders, he lost his footing and fell down a rocky 20-foot drop, fracturing both bones in his lower left leg, his wrist, both sides of his nose and his skull.A rescue squad carried him out of the woods, and a helicopter flew him to a pediatric hospital trauma unit in Roanoke.
Most of Christian's care was covered by his parents' insurance. But one bill stood out. Med-Trans, the air ambulance company, was not part of the family's health plan network and billed $36,000 for the 34-mile trip from the mountain to the hospital. It was greater than the cost of his two-day hospitalization, scans and cast combined.
"When you're in that moment, you're only thinking about the life of your child," says Christian's mother, Cynthia Bolling, an occupational therapist. "I know I'm being taken advantage of. It's just wrong."
The rising number of complaints about surprise medical bills is spurring efforts on Capitol Hill and at the White House to help consumers. Over and over again, the high cost associated with air ambulance service gives patients the biggest sticker shock — the subject has come up at nearly every Capitol Hill hearing and news conference on surprise medical bills.
Yet air ambulance costs are not addressed in any of the proposals introduced or circulating in Congress. Even a congressional decision last year to set up a panel that would study air ambulance billing hasn't gone anywhere.
"We're doing a disservice to patients if we protect them from hospital bills but bankrupt them on the way there," said James Gelfand, senior vice president for health policy for the ERISA Industry Committee, a trade association for large employers.
The issue came up again Wednesday at a House Energy and Commerce subcommittee hearing where Rick Sherlock, president and CEO of the Association of Air Medical Services (the industry group for air ambulances), was among eight witnesses.
Rep. Ben Ray Luján, D-N.M., sharply questioned Sherlock as to why costs for air ambulance services have risen by 300% in his state since 2006.
"I'm trying to get my hands around why this is costing so much and why so many of my constituents are being hit by surprise bills," Luján said.
Sherlock explained that reimbursements from Medicare and Medicaid do not cover the cost of providing services. So charges to private patients, he told the legislators, must make up that difference.
Air ambulances serve more than 550,000 patients a year, according to industry data, and in many rural areas, air ambulances are the only speedy way to get patients to trauma centers and burn units. As more than 100 rural hospitals have closed around the U.S. since 2010, the need has increased for air services.
More than 80 million people can get to a Level 1 or 2 trauma center within an hour only if they're flown by helicopter, according to Sherlock.
The service, though, comes at a cost. According to a recent report from the Government Accountability Office, two-thirds of the more than 34,000 air ambulance transports examined were not in the patients' insurance networks. That can leave patients on the hook for the charges that their insurers don't cover, a practice known as balance billing.
In 2017, the GAO found that the median price charged nationally by air ambulance providers was around $36,400 for helicopter rides and even higher for other aircraft. The total generally includes the costs for both the transportation and the medical care aboard the aircraft.
Additionally, the Bill of the Month investigative series by NPR and Kaiser Health News has received more than a dozen such bills, ranging from $28,000 to $97,000.
Cynthia Bolling says her insurance company paid about a third of Christian's air ambulance bill, and the family settled this week with Med-Trans, agreeing to pay $4,400 out of pocket.
Reid Vogel, director of marketing and communications for Med-Trans, says he can't discuss a particular patient's case because of privacy rules. But, he adds, Med-Trans works with patients to find "equitable solutions" when their bills are not covered by insurance.
Since nearly three-quarters of flights are for patients insured by low-paying Medicare, Tricare and Medicaid, he says, "providers must shift costs to insured patients."
Yet private insurers usually will pay only an amount close to what Medicare reimburses, which is around $6,500. That gives air ambulance companies an incentive to remain out of network, according to a 2017 GAO report.
"A representative from a large independent provider noted that being out of network with insurance is advantageous to the provider because a patient receiving a balance bill will ask for a higher payment from the insurance company, which often results in higher payment to the air ambulance provider than having a pre-negotiated payment rate with the insurer," the GAO found in its report.
Sherlock, of the air transport trade association, disputes the report's findings, saying his members are actively trying to be in network in more places, although he can't provide any specific numbers.
"I think that everywhere they can, they're incentivized to be in network," he says.
States are hampered in their efforts to ease the strain for residents.
The Airline Deregulation Act of 1978, which was intended to encourage more competition, prohibits states from regulating prices for any air carrier, including air ambulances. What's more, many large employers' health insurance is not governed by states but regulated by the federal labor law known as ERISA.
So a remedy likely has to come from Congress. And it has proved to be a heavy lift.
For example, the committees that deal with regulation of the air industry — the Commerce Committee in the Senate and the Transportation Committee in the House — don't make health policy or regulate health insurance.
Last year, some lawmakers sought to let states regulate air ambulances with a provision in the bill reauthorizing the Federal Aviation Administration.
But that measure was ultimately eliminated. Instead, the bill called for the creation of an advisory committee to study air ambulance prices and surprise bills.
"The air ambulance lobby did a very good job playing defense during FAA authorization," says Gelfand.
The panel, which was supposed to be formed within 60 days of the law's enactment date — Oct. 5, 2018 — still has not been created.
Representatives from the air ambulance industry don't think congressional action is necessary, although they are calling for higher reimbursements from Medicare.
Chris Eastlee, vice president for government relations at the Association of Air Medical Services, says his group does not favor more congressional regulation of prices but would support mandatory disclosure of costs to the secretary of the Department of Health and Human Services. Greater transparency, Eastlee's group argues, will help companies negotiate more in-network contracts.
A fix for surprise bills that is supported by some researchers and advocates would require every health care provider within a medical facility to accept any insurance plan that contracts with that hospital. It might also help bring down air ambulance bills, says Loren Adler, associate director of USC-Brookings Schaeffer Initiative for Health Policy.
It would avoid the situation where someone picks an in-network hospital only to find out that a surgeon or anesthesiologist at that hospital doesn't take the patient's insurance. Air transport should also be included in the rule, Adler says.
"It's the exact same situation as with the out-of-network emergency facility rates," Adler says. "The same solutions should apply."
Gelfand suggests also that the House Ways and Means Committee require air ambulance companies seeking to participate in Medicare to always charge in-network rates.
That would require only a small tweak of the legislative language, as Gelfand sees it. "Every proposal that includes something to address surprise bills for emergency care, all you [would] have to do is add in the words 'air ambulances,' " he says.
Right now, the closest any surprise-billing proposal has come to addressing air ambulances is a draft legislative plan on medical costs from Sen. Lamar Alexander, R-Tenn., and Sen. Patty Murray, D-Wash.
Their plan would require that bills for air ambulance trips be itemized to show both medical charges and the transportation charges — so patients and health plans can understand them better.
https://www.npr.org/sections/health-shots/2019/06/14/732174170/why-air-ambulance-bills-are-still-sky-high
Brand-name drug prices remain staggeringly high
by Diane Archer - Just Care - June 11, 2019
PharmacyChecker has released new information on brand-name drug prices in the US and around the globe. These drugs have no generic competition. And, the prices in the US remain staggeringly high relative to the rest of the world.PharmacyChecker looked at 10 popular brand drugs with no generic substitute. The savings from buying these drugs online from a verified pharmacy in Canada is 75 percent. Put differently, a drug that costs $100 in the US costs just $25 in Canada. Savings are even greater–a 90 percent discount–if you’re willing to buy your drugs from verified pharmacies in other parts of the world.
For example, Vesicare (solifenacin) treats overactive bladder (OAB). In the US, with a discount card, it costs $1,202 for 90 pills. In Canada it costs $188, 84 percent less. Discount cards are available for free from PharmacyChecker.com and GoodRx.
Of course, if you are considering importing drugs from abroad, you should know that it is prohibited under federal law. But, no one is ever fined, much less prosecuted, for importing drugs for personal use. If you opt to buy your drugs from abroad, as millions of Americans do, make sure you use a verified and properly credentialed pharmacy. Keep in mind that there are rogue online pharmacies that sell counterfeit drugs or just take your money.
Congress is currently considering legislation that would lower brand-name drug costs considerably. The most comprehensive and most fair legislation, the Prescription Drug Price Relief Act, was introduced by Congressman Ro Khanna and Senator Bernie Sanders. They propose that drug prices in the US be set at the average of what people in other wealthy countries pay for their drugs, international reference pricing.
https://justcareusa.org/brand-name-drug-prices-remain-staggeringly-high/?link_id=5&can_id=9f0819e2917760c9d722bd2e00c6077a&source=email-need-home-care-consider-moving-to-one-of-these-states&email_referrer=email_563504&email_subject=need-home-care-consider-moving-to-one-of-these-states
Drug Prices Are a Populist Campaign Issue. Here Are the Latest Proposals to Lower Costs.
by Katie Thomas - NYT - June 25, 2019
It can be hard to find common ground in Washington these days, but furor over drug prices could be one exception. Many Americans continue to struggle to pay for the prescription medicines they need. And rising drug costs are a problem for insurers and taxpayers, too — treatments for some rare diseases are topping $2 million.
As the presidential election heats up, politicians from both parties are eager to show they are doing something about a hot populist issue, and bipartisan solutions are beginning to take shape. Some proposals, like placing a limit on what older Americans must pay out of pocket for drugs, could make an immediate difference to people struggling with high costs. Others, like shutting down the games that pharmaceutical companies play to avoid competition, are more theoretical. They could streamline a complex system, but are unlikely to immediately lead to lower prices at the pharmacy counter.Here’s a guide to some of the proposals.
Use the power of the federal government to negotiate with drug companies.
Progressive Democrats have long argued that the federal government should be able to directly negotiate the price of drugs in Medicare, the health care program for older Americans. Under the current system, private insurers negotiate with the drug companies.Now, House Speaker Nancy Pelosi is said to be floating a compromise — one that would require the federal government to directly negotiate the price of about 250 expensive drugs a year. Under her proposal, which has not yet been introduced, the Department of Health and Human Services would negotiate with drug makers.
Companies that do not
comply could face a tax equal to half of that drug’s sales from the
previous year. Unlike some other plans, Ms. Pelosi’s proposal ensures
the same government-negotiated prices would be available to commercial
insurance plans.
Since a small number of drugs accounts for a major chunk of pharmaceutical spending, significantly lowering the price of even a few hundred drugs could go a long way toward lowering overall costs.
But whether her proposal will succeed is far from clear. The idea is likely to face opposition from many Republicans, who contend that private insurers are best equipped to negotiate with drug companies, and who may also be averse to imposing a steep tax on a major American industry.
Some progressive Democrats pushed Ms. Pelosi to expand the number of drugs that could be negotiated, from at least 25 drugs to the current 250. They favor an even broader plan that would affect all drugs.
Since a small number of drugs accounts for a major chunk of pharmaceutical spending, significantly lowering the price of even a few hundred drugs could go a long way toward lowering overall costs.
But whether her proposal will succeed is far from clear. The idea is likely to face opposition from many Republicans, who contend that private insurers are best equipped to negotiate with drug companies, and who may also be averse to imposing a steep tax on a major American industry.
Some progressive Democrats pushed Ms. Pelosi to expand the number of drugs that could be negotiated, from at least 25 drugs to the current 250. They favor an even broader plan that would affect all drugs.
Still, Ms. Pelosi’s plan should not be
discounted — her office is in talks with the White House over a drug
pricing deal that may include this proposal. President Trump has voiced
support for the idea of direct negotiation before.
The Trump administration’s plan would eliminate the legal protections for rebates, and require discounts to be passed along to consumers. Alex M. Azar II, the health and human services secretary, has said he hopes the change will simplify a broken system and give manufacturers an incentive to lower their list prices.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
But the true impact of the rule is far from clear, and the change could raise costs in other parts of the chain. While it would save some people money on out-of-pocket expenses, it is expected to raise drug-plan premiums for all Medicare beneficiaries, and it also would quite likely cost the federal government money. The nonpartisan Congressional Budget Office concluded in May that the rule, if adopted, would cost taxpayers $177 billion within 10 years.
The rule is also unusual because — unlike many other proposals to bring down drug costs — it is supported by the pharmaceutical industry, which has put part of the blame for rising prices on pharmacy benefit managers. Insurers and pharmacy benefit managers say the rule would stymie their ability to effectively negotiate with drug makers.
The Trump administration has signaled that it is likely to finalize the rule some time this year.
In addition, once a patient’s drug spending reaches a certain level in a year — $5,100 in 2019 — the federal government picks up most of the bill, rather than the private insurers who operate the drug plans.
Lower out-of-pocket costs for Medicare beneficiaries.
As one of the Trump administration’s major drug price initiatives, this proposal aims to reduce the costs that many older residents face at the pharmacy. Medicare consumers are often forced to pay out-of-pocket costs based on a list price, even when — behind the scenes — private pharmacy benefit managers have negotiated bigger discounts, or rebates, with the manufacturer.The Trump administration’s plan would eliminate the legal protections for rebates, and require discounts to be passed along to consumers. Alex M. Azar II, the health and human services secretary, has said he hopes the change will simplify a broken system and give manufacturers an incentive to lower their list prices.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
But the true impact of the rule is far from clear, and the change could raise costs in other parts of the chain. While it would save some people money on out-of-pocket expenses, it is expected to raise drug-plan premiums for all Medicare beneficiaries, and it also would quite likely cost the federal government money. The nonpartisan Congressional Budget Office concluded in May that the rule, if adopted, would cost taxpayers $177 billion within 10 years.
The rule is also unusual because — unlike many other proposals to bring down drug costs — it is supported by the pharmaceutical industry, which has put part of the blame for rising prices on pharmacy benefit managers. Insurers and pharmacy benefit managers say the rule would stymie their ability to effectively negotiate with drug makers.
The Trump administration has signaled that it is likely to finalize the rule some time this year.
Cap out-of-pocket spending under Medicare.
The drug coverage program known as Part D, for those who are 65 and older, has no limit on out-of-pocket spending. People who need expensive drugs (such as for cancer treatments or other serious diseases) can wind up paying thousands of dollars.In addition, once a patient’s drug spending reaches a certain level in a year — $5,100 in 2019 — the federal government picks up most of the bill, rather than the private insurers who operate the drug plans.
There
is some bipartisan support for capping out-of-pocket spending, as well
as for shifting more responsibility for the higher costs onto insurers
and drug makers. A proposal by House Democrats and Republicans
would limit annual out-of-pocket spending to $5,100. Senator Charles
Grassley, Republican of Iowa and chairman of the Finance Committee, has also expressed support for an out-of-pocket spending limit, as well as for shifting more of the financial responsibility to drug makers.
With members of both parties expressing support for this idea, it holds the promise of being one of the most significant moves that Congress could make this year to directly lower consumers’ drug costs.
The United States pays higher prices for drugs than any other country does, a situation that Mr. Trump describes as “global free-riding.”
The proposal is an unorthodox move for a Republican president, because it would effectively ride the coattails of countries with universal health care systems, such as France.
It is also fiercely opposed by an array of powerful lobbying interests, including the pharmaceutical industry — which described the proposal as “foreign price controls.” Health care providers also profit from the existing system and have opposed the proposal, warning that it could have “unintended consequences.”
The Trump administration may issue a proposal by the end of this year.
With members of both parties expressing support for this idea, it holds the promise of being one of the most significant moves that Congress could make this year to directly lower consumers’ drug costs.
Tie the price of some drugs to what they cost in other countries.
Another major proposal by the Trump administration would limit the price of some drugs covered by Medicare that are administered in a clinic or doctor’s office — expensive medications used for serious illnesses like cancer — by tying them to an index based on the price of the drugs in other countries.The United States pays higher prices for drugs than any other country does, a situation that Mr. Trump describes as “global free-riding.”
The proposal is an unorthodox move for a Republican president, because it would effectively ride the coattails of countries with universal health care systems, such as France.
It is also fiercely opposed by an array of powerful lobbying interests, including the pharmaceutical industry — which described the proposal as “foreign price controls.” Health care providers also profit from the existing system and have opposed the proposal, warning that it could have “unintended consequences.”
The Trump administration may issue a proposal by the end of this year.
Restrict the games drug companies play to avoid competition.
Drug companies love the word “innovation” when they talk about drug development, but they are also famously innovative in coming up with ways to shut down competitors.
Several
bills in Congress — many with bipartisan support — address the tactics
these companies use to maintain monopolies. Some proposals have passed the House
and have bipartisan support in the Senate, including one that would
force brand-name drug makers to turn over samples of their drugs to
would-be competitors so cheaper copies can be developed. Other measures
would limit the so-called “pay-for-delay” deals brokered by brand-name
drug companies and generic manufacturers to postpone competition.
Congressional observers say that of all the proposals, these have the best chance of becoming law. But while they are tweaks that make the existing system work more smoothly, they may not have a significant effect on prices.
Although the measure doesn’t directly reduce prices, Mr. Azar has said he hopes the move will shame drug makers into lowering them.
On Friday, three major drug makers — Merck, Eli Lilly and Amgen — filed a federal lawsuit seeking to block the rule, arguing that it violated their First Amendment rights and would mislead consumers.
https://www.nytimes.com/2019/06/16/health/drug-prices-congress-trump.html?smid=nytcore-ios-share
Congressional observers say that of all the proposals, these have the best chance of becoming law. But while they are tweaks that make the existing system work more smoothly, they may not have a significant effect on prices.
Require drug companies to list their prices in television ads.
The most visible step the Trump administration has taken to address drug costs is expected to be implemented this summer, when pharmaceutical manufacturers will be required to post in television advertisements the list price of drugs that cost more than $35 a month. (A disclaimer will note that patients covered by health insurance are likely to pay less.)Although the measure doesn’t directly reduce prices, Mr. Azar has said he hopes the move will shame drug makers into lowering them.
On Friday, three major drug makers — Merck, Eli Lilly and Amgen — filed a federal lawsuit seeking to block the rule, arguing that it violated their First Amendment rights and would mislead consumers.
https://www.nytimes.com/2019/06/16/health/drug-prices-congress-trump.html?smid=nytcore-ios-share
Washington and Hawaii rely on public funds to cover cost of home care for older adults
by Diane Archer - Just Care - June 12, 2019
Kaiser Health News reports on two states that have passed laws to help cover the cost of home care for older adults. Washington and Hawaii are relying on public funds to pay for long-term services and supports that enable more older adults to age in place.In Washington, a 0.58 percent payroll contribution will pay for a $36,500 long-term services and supports (LTSS) benefit under the Long-Term Care Trust Act. Everyone must pay this tax except self-employed people and people with private long-term care insurance. They can opt to pay in or not. The state government passed this new law after considering and rejecting the idea of strengthening commercial long-term care insurance.
The LTSS benefit begins in 2025 for people who pay in at least three years. Contributions will be collected beginning 2022. People who need help with at least three activities of daily living–bathing, dressing, toiletting, eating, and transferring– will be eligible for the benefit.
Up to $100 a day, adjusted for inflation, will cover home care and related services, including home modifications and respite care for family caregivers. It could also cover the cost of a wheelchair ramp or training a family caregiver on how to best care for someone with a particular condition. Washington authorities believe that the broader the range of covered services, the more likely older adults will be able to remain in their own homes.
The state projects Medicaid savings of $3.9 billion over 30 years. And, it predicts 15,000 residents will take advantage of the benefit in 2025. By 2052, they project 98,000 residents will use the LTSS benefit. Today, 66,000 residents get long-term supports and services through Medicaid.
In Hawaii, public funds pay for a caregiver program that covers $210 a week in home care services. The program restricts enrollment to people whose family caregivers work outside the home for at least 30 hours each week.
These two states’ innovative ways to help older adults age in place could be a model for the rest of the country. Nearly 100 million Americans will be 65 or older by 2050. And, the data suggests that the vast majority will not be able to afford long-term services and supports. But, as many as 70 million could need them.
Older adults often need help with bathing, feeding, toiletting, dressing and/or transferring from their bed to a chair. And, they typically need that help for two years. If they can stay out of nursing homes, they are not only likely to be happier, but it should save the government money.
Fewer than one in six Americans have long-term care insurance to cover the cost of LTSS. Those policies cost around $3,000 a year. And, it is not at all clear they are a good investment.
So far, the federal government has not passed legislation to cover long-term services and supports. Most recently, it tried to do so through the Affordable Care Act. The Community Living Assistance Services and Supports (CLASS) Plan, a provision of the ACA that was jettisoned, would have delivered as much as $50 in daily benefits for home care or nursing home care. It was a voluntary government insurance program that would have charged people a premium.
For now, several states are looking into a variety of ways to help their residents age in place. In Minnesota, the state may let people convert life insurance policies to long-term care insurance. In Maine, the state is promoting long-term care insurance. Mainers recently voted against a ballot proposal to provide free long-term care to residents. It would have been paid through a 3.8% income tax on people with annual incomes above $128,400.
In California, Michigan and Illinois, state long-term services and support programs are also under consideration. Over the years, the New York State Assembly has passed a bill that would increase income taxes to pay for LTSS. But, the New York State Senate has not passed it.
https://justcareusa.org/washington-and-hawaii-rely-on-public-funds-to-cover-cost-of-home-care-for-older-adults/?link_id=1&can_id=9f0819e2917760c9d722bd2e00c6077a&source=email-need-home-care-consider-moving-to-one-of-these-states&email_referrer=email_563504&email_subject=need-home-care-consider-moving-to-one-of-these-states
As price of insulin soars, Americans caravan to Canada for lifesaving medicine
by Emily Rauhala - Washington Post - June 16, 2019
As their minivan rolled north, they felt their nerves kick in — but they kept on driving.
At the wheel: Lija Greenseid, a rule-abiding Minnesota mom steering her Mazda5 on a cross-border drug run.
Her
daughter, who is 13, has Type 1 diabetes and needs insulin. In the
United States, it can cost hundreds of dollars per vial. In Canada, you
can buy it without a prescription for a tenth of that price.
So,
Greenseid led a small caravan last month to the town of Fort Frances,
Ontario, where she and five other Americans paid about $1,200 for drugs
that would have cost them $12,000 in the United States.

Pharma companies have raised prices for new drugs and commonly
used medications, prompting many patients to order medications across
the border.
(Luis Velarde/The Washington Post)
“It felt like we were robbing the
pharmacy,” said Quinn Nystrom, a Type 1 diabetic who joined the caravan
that day. “It had been years since I had 10 vials in my hands.”
They’re
planning another run to Canada this month to stock up on insulin — and
to call attention to their cause. This time, they’ll be taking the
scenic route, driving from Minnesota through Wisconsin, Illinois, and
Michigan en route to London, Ontario, where Frederick Banting began the
work that led to the discovery of insulin nearly a century ago.
Like millions of Americans, Greenseid and Nystrom are stressed and outraged by the rising costs of prescription drugs in the United States — a problem Republicans and Democrats alike have promised to fix.
Insulin is a big part of the challenge. More than 30 million Americans have diabetes, according to the American Diabetes Association. About 7.5 million, including 1.5 million with Type 1 diabetes, rely on insulin.
Between 2012 and 2016, the cost of insulin for treating Type 1 diabetes nearly doubled, according to the nonprofit Health Care Cost Institute.

Some
pharmaceutical companies, under pressure from U.S. lawmakers, have
tried to reduce the cost for some patients. But many who rely on insulin
still struggle. Large numbers resort to rationing — a dangerous and sometimes deadly practice.
Some
diabetics and their families are taking matters into their own hands.
They meet in coffee shops and strip mall parking lots to exchange
emergency supplies. An unknown number travel outside the country to buy
the lifesaving drug for less.
None of this is recommended by U.S. officials, and some of it might be illegal
under Food and Drug Administration guidelines. But the organizers of
the caravan — their word, a nod to the migrants traveling in groups
through Mexico to the U.S. border — are speaking out about their trip
because they want Americans to see how drug prices push ordinary people
to extremes.
“When you have a bad health-care system, it makes good people feel like outlaws,” Greenseid said.
“It’s demeaning. It’s demoralizing. It’s unjust.”


Lija Greenseid and her 13-year-old daughter at their home. (Jenn Ackerman for The Washington Post)
The caravaners aren’t the only ones looking north. Republicans and Democrats have produced federal and state proposals to import drugs from Canada.
Those
ideas aren’t necessarily popular in Ottawa, where many worry that bulk
buys from the United States could cause shortages or higher prices.
Barry
Power, director of therapeutic content with the Canadian Pharmacists
Association, said the group is tracking both U.S. drug-buying proposals
and reports of cross-border trade closely but has yet to see a
disruption to Canadian insulin supplies.
He said insulin prices in Canada are controlled through policy, including price caps and negotiations with manufacturers.
“This is something the U.S. could do,” he said.
When Banting co-discovered insulin in the early 1920s, he balked at commercializing it because it seemed unethical to profit from a critical drug. He eventually sold his share of the patent to the University of Toronto for $1, in the hope the drug would remain widely accessible.
In
the nearly 100 years since, insulin has become a lifeline for millions.
But the price in the United States has surged in ways its discoverers
could not have predicted.

Quinn Nystrom, a Type 1 diabetic, with her parents in Eveleth, Minn. (Courtesy of Quinn Nystrom)
When
Nystrom was diagnosed with diabetes as a child in the late 1990s, she
said, her family paid about $15 to $20 a vial. Now, at 33, she sometimes
pays more than $300 for the same amount.
Nicole
Smith-Holt, who drove north with Greenseid and Nystrom, said her son
spent about $1,000 per month on the drug. Alec Raeshawn Smith, an
uninsured Type 1 diabetic, rationed his insulin supply due to cost, his mother said. He died in 2017.
Elizabeth
Pfiester is founder and executive director of T1International, a
British-based nonprofit that advocates for people with Type 1 diabetes
around the world.
“It’s kind of a myth that
America has the best health-care system in the world, because it is set
up to allow Americans to go bankrupt or die because they can’t afford
their medicine,” she said.
Pfiester grew up in
the United States. One of the reasons her organization is based
overseas, she said, is that the cost of treating her diabetes in the
United States is so high.
“What I think is
quite clear is that these companies will charge what they can get away
with,” she said. “They have been able to get away with costs going up
because of a broken and opaque health-care system.”
A
spokeswoman for the Pharmaceutical Research and Manufacturers of
America noted that drug companies are increasingly offering rebates on
insulin in the United States — but they aren’t always reaching
consumers.
“Too often, these negotiated
discounts and rebates are not shared with patients, resulting in the
sickest patients paying higher out-of-pocket costs to subsidize the
healthy,” PhRMA spokeswoman Holly Campbell said in an email. “This is
the opposite of how health insurance is supposed to work.”
Greenseid,
who has purchased insulin for her daughter in six countries, said U.S.
prices stand out as not just high, but as unpredictable. As people
bounce between insurance plans and navigate rebates, she said, you often
“have no idea how much you are going to pay.”
In the United States, you can buy some types of insulin without a prescription. But to get the newer analog insulin on which Type 1 diabetics rely, you need to visit or call your doctor.
If
Nystrom forgets to pack enough for an extended trip, she said, she
needs to get her endocrinologist on the phone. In Canada, she can walk
into a pharmacy and get the analog insulin she needs.
“The attitude up there is: ‘Why would someone buy insulin if they didn’t need it?’ ” Nystrom said.
On
their first trip north, the caravaners received support from Canadians,
they said, but also accusations that they were looting drug supplies.
“We heard a lot of comments like, ‘Canada needs to put up a wall,’” Smith-Holt said. “I was like, ‘Oh, come on.’ ”
Before
the group set out for Fort Frances, they said, they called ahead to
check that the local pharmacy had enough to fill their order without
disrupting supply.
They see buying in Canada as a short-term emergency measure and a way to call attention to U.S. pricing — not the answer.
“I
don’t think that the solution is going outside the United States,”
Greenseid said. “The reason they have lower prices is because they have
put in regulations to make sure their citizens are not paying too much.
We have not yet made that decision in the U.S.”
LaShawn McIver is senior vice president for government affairs and advocacy at the American Diabetes Association.
“Insulin
is not a luxury, it is a matter of life and death,” she wrote in an
emailed statement. “Action to reduce the high out-of-pocket costs that
endanger the lives of the millions of Americans who depend on this
medication is critical and urgently needed.”
A
spokeswoman for the Department of Health and Human Services, which
oversees the FDA, said the Trump administration is focused on lowering
drug prices.
“President Trump and [Health AMD
Human Services] Secretary [Alex] Azar are firmly committed to getting
drug prices down,” spokeswoman Caitlin B. Oakley wrote in an email.
“They are both very open to the importation of prescription drugs as
long as it can be done safely and can deliver real results for American
patients.”
Until things change, the caravaners say, they’ll keep driving.
Their
first trip led to queries from families across the country, they said,
including Type 1 diabetics, parents of children with diabetes and family
members supporting elderly relatives with diabetes. Some want to join.
So when they head north in a few weeks, they’ll switch from family cars to a chartered bus.
Boston drug-pricing watchdog group has pharma companies’ attention - The Boston Globe
by Shirley Leung - Boston Globe - June 20, 2019
Two days later the drug, Zolgensma, won approval. Novartis priced it at a jaw-dropping $2.1 million, still the most ever for a medicine. Pearson’s group didn’t object, agreeing that the one-time, life-saving treatment for spinal muscular atrophy — the leading genetic killer of infants — might be worth that much.
Get Talking Points in your inboxAn afternoon recap of the day's most important business news, delivered Monday through Friday.
It
marked just the latest effort by the Institute for Clinical and
Economic Review — a name only a policy wonk could love — to get drug
firms to charge only what it says a medicine is worth. ICER researchers
spend about eight months studying how well a medicine works and whether
it might reduce other health care costs, then publicize their findings
in the hopes of getting drug makers to set a fair price.In the past two years or so, the nonprofit persuaded a partnership of two drug firms to charge far less for an injectable eczema treatment than analysts had expected; pressured the same partnership and a third firm to cut the costs of two competing cholesterol-lowering drugs; and saw the Department of Veterans Affairs adopt the institute’s pricing guide for medicines prescribed to military veterans.
Pearson, a doctor with a master’s degree in health policy and management from Harvard University, acknowledges that pharmaceutical firms continue to wield enormous power and that ICER can only offer opinions — it has no regulatory authority. Still, the group is gaining clout as more Americans blanch at dizzying drug prices.
“We’re the mouse that roared,” Pearson, 59, said in his spartan ninth-floor office in Liberty Square. ICER, he said, stands up to “huge companies, huge resources, huge everything,” in an attempt to rein in spiraling health costs.
The group is also making enemies. Drug makers, pharmaceutical lobbyists, and some self-described patient advocacy groups say the institute threatens to stifle innovation and could make some medicines unavailable, if insurers agree they are overpriced and limit who can get them.
Cambridge-based Sarepta Pharmaceuticals refuses to help the institute’s researchers evaluate its medicines, and Boston-based Vertex Pharmaceuticals says it did help but won’t again. Drug firms typically assist ICER by providing research material, such as unpublished data on the benefits of a drug.
Sarepta and Vertex executives say the institute’s pricing model is biased against drugs for deadly rare diseases, the focus of their businesses. Those medicines can cost six figures or more because they are expensive to make and treat relatively few patients, the companies say.
“We refused to participate because we knew exactly where ICER would end up with this and similar rare-disease drugs,” Douglas Ingram, CEO of Sarepta, said of a recent review of his firm’s medicine to treat Duchenne muscular dystrophy, a deadly rare muscle-wasting disease that mostly affects boys.
The medicine, Exondys 51, won a controversial approval from the Food and Drug Administration in 2016 and carries a list price of $892,000 a year, even though an FDA advisory panel questioned whether it works. Last month, ICER said in a draft report that the drug was of such marginal value that the institute couldn’t even put a price tag on it. Ingram dismissed the institute’s finding as “preordained.”
Terri Ellsworth, whose 18-year-old son, Billy, began participating in a clinical trial of Exondys when he was 10 and has taken the drug ever since, said he would need a wheelchair if not for the weekly infusions. He graduated from his suburban Pittsburgh high school this month and was able to walk on stage to get his diploma.
“Ask the patients if the benefits are marginal,” his mother said. “When I first saw this [ICER] report, I thought, ‘Who are these people and who are they working for?’ To me, it’s clearly the insurance companies.”
Pearson denies that, and several doctors, insurance executives, and health policy experts agree.
They say the health care system, including state Medicaid agencies such as MassHealth, can’t afford a stream of drugs whose prices rival the cost of a house. At the least, they say, the system needs an umpire to say whether the medicines are worth it.
“ICER is filling that gap,” said Michael Sherman, a physician and chief medical officer for Harvard Pilgrim Health Care, the second-largest private insurer in Massachusetts. “As we come to the realization that we don’t have an unlimited global budget, it becomes more important to have some objective metric that we can point to.”
Sherman sits on an 18-member board that advises the institute. It includes physicians, economists, and executives from pharmaceutical firms and insurers.
Prescription drug prices have sparked a populist furor in recent years. The US government, unlike those of most other developed countries, sets no ceiling on what pharmaceutical companies can charge. The only limit is what the market will bear.
Pearson founded the institute in 2006. A San Diego native, he earned his medical degree at the University of California San Francisco and completed his residency in internal medicine at Brigham and Women’s Hospital in Boston.
He spent a year at the National Institute for Health and Care Excellence, a government agency in the United Kingdom that approves drugs and decides what they should cost. He also served as an adviser to the Centers for Medicare and Medicaid Services under President George W. Bush.
ICER initially focused on the clinical value and cost effectiveness of medical technology, such as robotic surgery for prostate cancer. It turned to drugs in 2014 soon after the FDA approved Sovaldi, Gilead Sciences’ blockbuster cure for hepatitis C. Although remarkably effective, Sovaldi ignited a firestorm because of its list price of $1,000 per pill — a total of $84,000 for a course of treatment.
That’s cheap compared with Zolgensma and other new drugs, but it prompted ICER to scrutinize dozens of other medicines to gauge a reasonable cost.
“We don’t have any power to make that stick,” said Pearson, but ICER can say, “Here’s what the evidence says about the effectiveness of your treatment and what a fair price aligned with that would look like.”
The institute has about 30 employees and a budget of about $7 million. Some 77 percent of its funding comes from donations by nonprofits, according to ICER’s website. And most of that comes from the billionaire Houston philanthropic couple John and Laura Arnold, critics of soaring health care costs. The remaining 23 percent comes from drug makers, health insurers, and the Medicaid departments of several states.
Pearson’s total compensation in 2017 was $481,846, according to ICER’s most recent filing with the Internal Revenue Service.
To measure the value of a medical treatment over time, ICER uses a unit employed by health economists: “quality-adjusted life year,” or QALY. One QALY (pronounced “kwaly”) equals a year of perfect health as a result of a medicine. Zero QALYs equals death.
A medicine that adds a year of perfect health to a life is worth $100,000 to $150,000, the institute says, citing data from the World Health Organization and other sources.
Using this calculation, the institute has studied more than 75 brand-name drugs. It determined that roughly two-thirds are overpriced, even though some are considered medical breakthroughs.
They include three drugs that Boston-based Vertex has introduced since 2012 to treat cystic fibrosis, a rare genetic illness that attacks the lungs and other organs. The list prices of those drugs — Kalydeco, Orkambi, and Symdeko — range from $273,000 to $312,000 annually. ICER said last year that Vertex would have to lower its prices by 71 to 77 percent to align costs with benefits.
In a letter to Pearson, Samantha Ventimiglia, Vertex vice president for government affairs and public policy, called the analysis a “sham.” She said it relied on a “flawed scientific methodology” and could limit patients’ access to “transformative and life-saving medicines,” if insurers agreed with the institute.
Among ICER’s most outspoken critics is Robert K. Coughlin, who leads the Massachusetts Biotechnology Council trade group.
His son, Bobby, was born with cystic fibrosis and will be a senior at Dedham High School in the fall. Bobby hopes Vertex will soon win approval of a drug that targets his particular mutation. The elder Coughlin seems offended by the idea of calculating a “fair price” for a treatment that could save his son’s life.
“This isn’t just like a business transaction,” he said. “How do you put a price tag on someone’s life?”
Such arguments may resonate on an emotional level, but they overlook that the nation cannot continue to afford rising drug costs, said Dr. Peter Bach, head of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center in New York.
The average American spent $134 a year on prescription drugs in 1980 compared with $1,025 by 2017, when adjusted for inflation, Bach said, citing a study by the Kaiser Family Foundation. He said drug companies should be rewarded for developing life-saving treatments, but “that shouldn’t mean they can charge an infinite amount.”
Pearson said ICER isn’t out to get drug makers any more than it’s seeking to boost health insurers. It just wants fair drug prices.
“We’re not here to tell the pharmaceutical industry that they’re evil,” he said. “We’re not here to tell the payers that they’re evil. We’re here to find the win-win by providing an independent look at the evidence.”
https://www.bostonglobe.com/business/2019/06/19/boston-drug-pricing-watchdog-group-has-pharma-companies-attention/opfu6zAa3TKecdshGc2hsI/story.html?et_rid=1744895461&s_campaign=todaysheadlines:newsletter
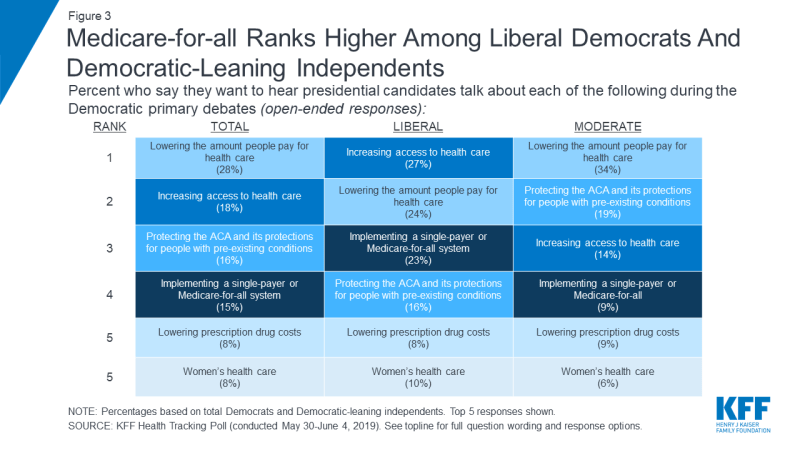
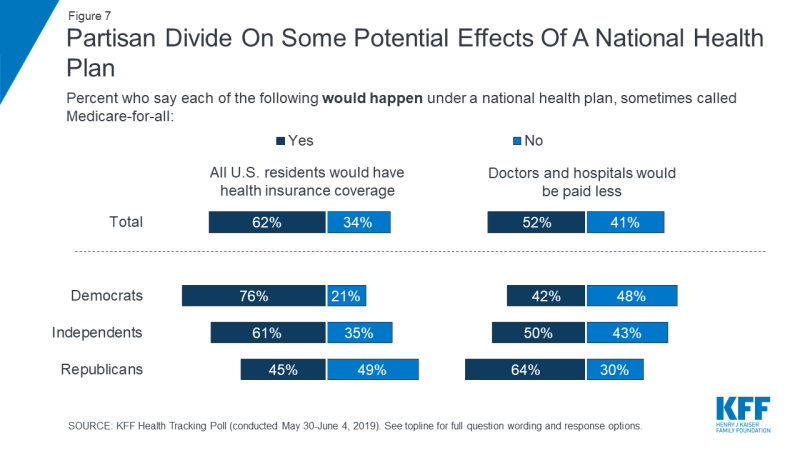
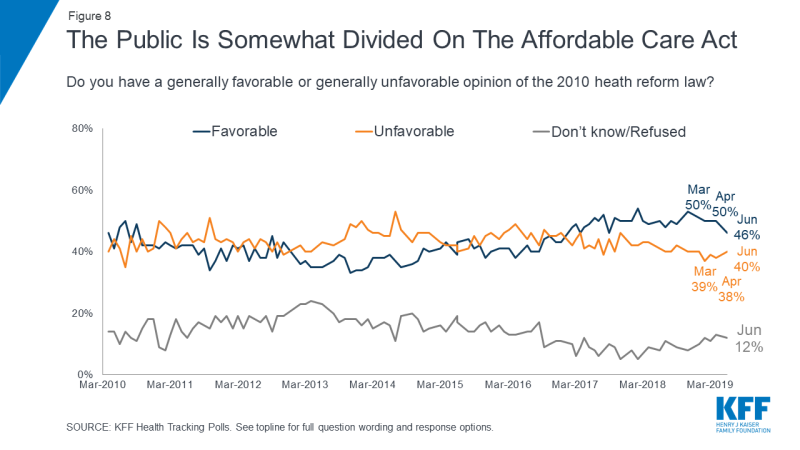
No comments:
Post a Comment